- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Study Casts Doubt on Angioplasty, Bypass for Many Heart Patients
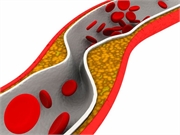
Bypass operations, angioplasty and the placement of artery-opening stents: For decades, millions of Americans have undergone these expensive, invasive procedures to help treat clogged vessels.
However, the results of a large and long-awaited clinical trial suggests that, in most cases, these procedures may not have provided any benefit over medications and lifestyle changes.
In fact, people treated with meds and healthy changes in lifestyle wound up about as healthy as those who underwent an invasive procedure to open their hardened arteries, researchers reported Saturday at the American Heart Association (AHA) annual meeting in Philadelphia.
Only a subgroup of patients who suffered from frequent angina appeared to receive any benefit from an invasive procedure, and that benefit was in their quality of life, not in lowering their odds of death or future heart problems.
“Based on the trial results to date, I as a clinician would feel comfortable advising my patient not to undergo the invasive strategy if their angina was absent or controlled or it was tolerated,” said Dr. Alice Jacobs, director of the Cardiac Catheterization Laboratory and Interventional Cardiology at Boston Medical Center. She wasn’t involved in the new research.
Still, doctors are often uncomfortable limiting their treatment of clogged arteries to drugs, diet and exercise alone because they’re worried the patient will wind up suffering a heart attack or other heart-related illness, according to past AHA president Dr. Elliot Antman.
The new findings are expected to give physicians more confidence in saying no to invasive treatments, the experts said.
The study did not focus on people who are admitted to a hospital with a heart attack — these patients often receive bypass, angioplasty or stenting to quickly open a blocked artery.
Instead, the trial focused on patients with stable but severe heart disease.
A typical patient in this group might be a 71-year-old grandmother who has noticed during the past two months some chest heaviness walking from the parking lot to her grandkids’ soccer game, the AHA presenters said. Stress testing and imaging scans could reveal some moderately clogged arteries leading to her heart.
The new trial was very comprehensive, involving nearly 5,200 patients across 37 countries. Half were randomly assigned to undergo an invasive procedure: About three-quarters underwent angioplasty (most receiving a stent as well), while the others had a bypass operation.
The other half of patients were treated with medications and lifestyle changes alone.
Researchers mainly focused on whether the invasive procedure would reduce a patient’s risk of heart-related death, heart attack, hospitalization with unstable angina, heart failure or cardiac arrest.
Overall, an invasive strategy “did not demonstrate a reduced risk over a median 3.3 years” compared with the more conservative, drugs/lifestyle therapy, said trial co-chair Dr. Judith Hochman, a cardiologist and senior associate dean of clinical sciences at NYU Langone Health, in New York City.
However, invasive procedures did have a positive impact on one patient subgroup: People who regularly suffer the chest pain and shortness of breath associated with angina, said co-researcher Dr. John Spertus. He directs health outcomes research at Saint Luke’s Mid-America Heart Institute in Kansas City.
“For a patient who has weekly angina, there would be 15% of them who would be expected to be angina-free with the conservative approach, while 45% would be expected to be angina-free with the invasive approach,” Spertus said. “This is such a large difference that you would only have to treat about three patients with weekly angina for one to be angina-free at three months.”
On the other hand, patients who did not regularly have angina received only minimal quality-of-life or symptom benefits after undergoing an invasive procedure, Spertus added.
A smaller set of trials — this time focused on patients with chronic kidney disease — revealed even less promising results, researchers said. Patients didn’t gain any health benefits and didn’t have any improvement in their quality of life after getting an invasive treatment. Angioplasty might even help put them on dialysis earlier or increase their risk of stroke, the study found.
Dr. Glenn Levine, a professor of cardiology with Baylor College of Medicine in Houston, said that when it comes to kidney patients with clogged arteries, he “will treat them with medical [drug] therapy alone” unless they have marked or uncontrolled angina.
Experts said the main message from these studies is that doctors shouldn’t feel pressured to immediately send patients with clogged arteries into a catheterization lab, especially if they aren’t suffering any symptoms.
That could free up physicians to focus on getting patients to take their medications, Jacobs said. If drug therapy helps relieve their occasional angina or other symptoms, then angioplasty might be avoided in two out of every three patients, she estimated.
The trials were funded by the U.S. National Heart, Lung, and Blood Institute.
For more information:
There’s more on common heart procedures at the American Heart Association.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










