- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
- How Daily Prunes Can Influence Cholesterol and Inflammation
- When to Take B12 for Better Absorption and Energy
Pandemic to Endemic: Is a New Normal Near?
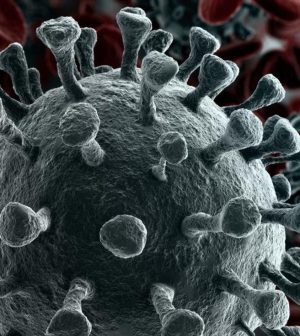
It has begun to feel like a pandemic that will never end, but public health experts now say the Omicron variant may be ushering in a “new normal,” where COVID-19 becomes an endemic, but manageable, disease.
“I do feel that we are moving into a transition phase in the pandemic, and I do think Omicron represents a major move to endemicity,” Dr. Christopher Woods, a Duke professor of medicine, pathology and global health and chief of the infectious diseases division at the Durham VA Medical Center, said during a Duke University media briefing on Monday that focused on the pandemic. “That’s my optimistic outlook at the moment.”
That’s because the latest surge in cases has turned out to be less deadly, he noted, at least among those who have been vaccinated and/or boosted.
So the surge “will augment population immunity,” Woods added. And with Omicron case counts now easing in much of the United States, he predicts fewer infections in the spring and summer, absent the arrival of any new problematic variants.
That’s good news as the pandemic moves into its third year.
“None of us, even those of us who wrote about this, could have imagined we would now be going into the third year of the first global and really devastating pandemic of the 21st century,” Dr. Jonathan Quick, a professor at Duke, said during the briefing.
Quick is an adjunct professor with the Duke Global Health Institute and managing director of pandemic response, preparedness, and prevention with the Rockefeller Foundation.
Quick noted the “stunning” nature of the first two years, as the new coronavirus shape-shifted through one new threatening variant after another.
Still, Quick firmly believes that now “we have the tools to stop COVID-19 as a global pandemic.”
However, he added, “What this new normal looks like, and how quickly we get there, will basically depend on two things: One is what the virus does — and so far it has been predictably unpredictable — and what humans do.”
What comes next?
“We’re already on the path with the tools we have,” said Quick, who laid out three possible future scenarios.
One is total disease eradication, something that’s only been achieved once — with smallpox.
The second is elimination of most — though not all — outbreaks, something that was almost achieved early this century in the fight against measles.
And the third is a gradual shift away from a full-blown threat to an endemic disease that humans learn to live with.
Even so, that won’t mean a COVID-free world, Woods stressed.
For one, he sees a transition to seasonal peaks, where infection risk likely goes up during winter “as with influenza.” That means “annual boosters will almost surely be needed, and vaccines will most likely need to be periodically updated,” Woods noted.
Another Duke expert said vaccines have made the difference, and will keep doing so in the future.
“There is no doubt in my mind that vaccines will continue to play a central role in our fight against COVID-19 as we transition to an endemic phase,” said Lavanya Vasudevan, an assistant professor in Duke’s department of family medicine and community health and the Global Health Institute.
It’s “frightening,” she added, “to think about how much higher the toll would have been without these vaccines.”
But even as vaccines plus natural immunity drive the move towards a “new normal,” Vasudevan warned there are still big hurdles ahead.
On the one hand, COVID fatigue gives rise to complacency and drives down vaccination rates. And in light of continued vaccine resistance and misinformation, she said it will be critical to stay focused “on messaging around the importance of vaccines.”
Vaccines will need a revamp
New vaccines geared for children under 5 will also be needed, Vasudevan added.
And both she and Quick stressed that while vaccines have been a game-changer, the ones on hand are still not good enough for the long haul.
While acknowledging that “we’re going someplace where no public health program has gone before with the level of vaccination that’s needed,” Quick cautioned that, “we’re not going to be able to maintain vaccination protection… if we have to have to have a booster every six or even 12 months.”
So, “now we really need an approach to get the best possible vaccine,” Quick added.
“The reality is that we still don’t have a clear sense of the durability of the vaccines we have. If people are hoping that once Omicron, as it appears to be doing, drops off and comes back to the relatively low level we were six months ago, there’s going to be a tendency to say, ‘OK, let’s back off,'” he said. “But given our evolving knowledge about the durability of the vaccines we have, and given our need to really make a much more concerted effort towards new vaccines that cover a wider range of coronaviruses, we need to stay on the alert. It would be six-to-12 months before I would be comfortable saying we may be out of the woods.”
Beyond that, both Vasudevan and Woods believe that masks are likely here to stay, at least for a while.
“Count me among those who don’t enjoy wearing masks,” admitted Woods. “But it feels that it is my duty to protect others, both inside and outside the hospital.”
That imperative, he said, means that masks will probably remain a fact of life in health care settings, as well as when flying or using mass transit, though he believes their use “will wax and wane with the epidemic information our surveillance system feeds us.”
Ensuring that surveillance system is strong will be hugely important, all three Duke experts agreed, so that the public has a real-time sense of how to behave as the world shifts towards living with the virus.
It’s important to “stay on the alert,” said Quick, who added that lessons can be drawn from the 1918 flu pandemic. At that time, “we had a fourfold difference in the death rate in cities around this country,” he noted. “And the thing was those places that let their guard up too early, relaxed their protective measures too early, were the ones that were hit the hardest.”
To prevent that, Quick envisions the establishment of a public early warning system that is in some ways analogous to weather prediction.
“We have reduced weather-related deaths by 95% over the last five decades by being able to pick up the warnings,” he noted. “Now, when there’s a hurricane coming … most people will change their behavior appropriately. That’s what we need to do.”
More information
There’s more on the endemic future of COVID-19 at the Harvard School of Public Health.
SOURCES: Jan. 24, 2022, Duke media briefing with: Jonathan Quick, MD, MPH, adjunct professor, Duke Global Health Institute, Durham, N.C., and managing director, pandemic response, preparedness, and prevention, Rockefeller Foundation, and senior fellow, Management Sciences for Health; Christopher Woods, MD, professor, medicine, pathology and global health, and co-director, Hubert-Yeargan Center for Global Health, Duke University, Durham, N.C., and chief, infectious diseases division, Durham VA Medical Center; Lavanya Vasudevan, PhD, assistant professor, department of family medicine and community health and the Global Health Institute, Duke University, Durham, N.C.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










