- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
- How Daily Prunes Can Influence Cholesterol and Inflammation
Incontinence Surgery Bests Physical Therapy in Trial
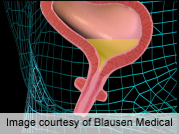
WEDNESDAY, Sept. 18 Stress urinary incontinence is a common problem among women, and new research suggests that surgery might be a better first-line treatment than pelvic muscle strengthening.
In what is billed as a first comparison of the two therapies, Dutch researchers found that almost 91 percent of women who had a type of surgery called midurethral-sling surgery reported improvement compared to 64 percent of women who had physical therapy for pelvic floor muscle training to correct the problem.
“The prevalence of stress urinary incontinence — leakage on physical exercise, laughing, coughing — is high, and the impact on daily life can be substantial,” said study lead author Dr. Julien Labrie, a gynecology resident at the University Medical Center Utrecht, in the Netherlands.
“Regardless of the severity of the incontinence, pelvic floor muscle training is the first-line treatment in most international guidelines,” Labrie said. “With rapidly increasing evidence that [midurethral-sling surgery] is safe with lasting efficacy, we believed it was time to compare surgery with pelvic muscle floor training as a first-line treatment for women with moderate to severe stress urinary incontinence.”
Results of the study are published in the Sept. 19 issue of the New England Journal of Medicine.
Stress incontinence is a problem that affects many women as they age, and it has a negative affect on quality of life, according to the National Association for Continence.
The treatment options include pelvic muscle floor training, which involves exercises known as kegels that help strengthen the pelvic muscles. The hope is that the stronger muscles can effectively close the urethra, holding back urine. The rates of subjective success vary greatly for pelvic muscle floor training — from 53 percent to 97 percent, according to background information in the study.
There also are several surgical options. One is the midurethral-sling surgery, which is a minimally invasive procedure that involves inserting a hammock-like device underneath the urethra to give it additional support and compression to help it stay closed. Subjective cure rates for this procedure vary from 75 percent to 94 percent, the study reported.
To see how these options compared, the researchers recruited 230 women for pelvic muscle floor training (physiotherapy) and another 230 for surgery. The researchers allowed the women in either group to switch if they were unhappy with their treatment.
Nearly half of the women in the physiotherapy group switched to the surgical group, while 11 percent of the women in the surgery group crossed over to physiotherapy during the study.
After a year, the researchers found that subjective improvement was reported by 90.8 percent of the women in the surgery group and 64.4 percent in the physiotherapy group. The rates of subjective cure were somewhat lower — 85.2 percent for those in the surgical group and 53.4 percent for the physiotherapy group.
Risks of surgery include perforation, the need for reoperation, postoperative bleeding, blood loss and new urinary urge incontinence, according to the study.
“We feel surgery and physiotherapy should both be offered as first-line treatment options,” Labrie said. “The woman herself should be involved in deciding what, in her individual case, should be the treatment.”
Labrie noted, however, that the trial did not include women with mild incontinence, so the results shouldn’t be applied to women who have mild stress incontinence.
Dr. Benjamin Brucker, an assistant professor of female pelvic medicine and reconstructive surgery at the NYU Langone Medical Center in New York City, called the study “very well designed.”
The data on surgical complications was reassuring because the complications were relatively minor, he said.
But where does all this leave women who have urinary incontinence? What option should they choose?
“Each woman is unique,” Brucker said. “What works best for one woman isn’t what would work best for every other woman.”
“On an individual level, this study shows that if you want to be conservative, you don’t lose anything by having physiotherapy first,” he said. “But it also shows that depending on your embarrassment and emotional health scores, if you’re a woman who says, ‘I just want to put this behind me,’ you’re not doing yourself a disservice by having surgery first.”
More information
Learn more about stress incontinence and treatment options from the National Association for Continence.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










