- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
Certain Thyroid-Related Diseases May Vary by Race

Race appears to be a factor in determining a person’s risk of developing autoimmune thyroid conditions such as Graves’ disease or Hashimoto’s thyroiditis, a new study says.
African Americans and Asians are much more likely to develop Graves’ disease than whites are, according to the study published in the April 16 issue of the Journal of the American Medical Association.
On the other hand, whites have an increased risk of Hashimoto’s thyroiditis when compared to other ethnic groups, the researchers found.
The findings are based on analysis of medical records from all United States active duty military personnel aged 20 to 54 from 1997 through 2011.
“These stark race differences in the incidence of autoimmune thyroid disease raise the important question of why?” said lead author Donald McLeod, an endocrinologist and researcher at the QIMR Berghofer Medical Research Institute in Queensland, Australia. “If we can work this out, we may unlock the mechanisms of autoimmune thyroid disease, and potentially yield insights into other autoimmune disorders.”
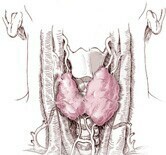
The thyroid gland plays a crucial role in regulating the body’s metabolism, influencing how quickly a person burns calories, how fast their heart beats, and how alert they feel.
Graves’ disease occurs when the immune system begins producing an antibody that tricks the thyroid into producing too much hormone. It’s the most common cause of hyperthyroidism, and affects about one in every 200 people, according to the U.S. National Institutes of Health (NIH).
Hashimoto’s thyroiditis happens when the immune system attacks the thyroid gland itself, causing hormone production to fall and causing hypothyroidism. Hashimoto’s affects as many as 5 percent of adults, according to the NIH.
Both conditions are chronic illnesses but can be treated with medication. Left untreated, people with Graves’-related hyperthyroidism can become nervous or irritable and suffer hand tremors, a rapid and irregular heartbeat, and weight loss. Hypothyroidism caused by Hashimoto’s has almost the opposite effect on the body, causing people to experience fatigue, difficulty concentrating, a slowed heart rate and mild weight gain.
The analysis found that, compared to whites, black women are about twice as likely and black men are about two and a half times more likely to have Graves’ disease.
Asian/Pacific Islander women had a 78 percent increased risk of Graves’ disease compared to whites, while Asian/Pacific Islander men had a more than threefold increased risk, the study noted.
But the risk of Hashimoto’s in both blacks and Asian/Pacific Islanders was much lower than the risk among whites, ranging from 67 percent to 78 percent less, the findings showed.
“The findings are striking, that there are so many more African Americans and Asian individuals who are coded as having Graves’,” said Dr. James Hennessey, director of clinical endocrinology at Beth Israel Deaconess Medical Center in Boston. He was not involved with the new research.
Study author McLeod demurred when asked about how a person’s race could influence their thyroid function.
“Our current study can’t answer whether racial differences in autoimmune thyroid disease incidence are due to genetics, environmental exposures or a combination of both,” McLeod said. “Further work needs to be performed to find the underlying mechanisms of thyroid autoimmunity.”
In the paper, the researchers rule out one potential environmental influence — smoking.
Smoking is associated with an increased risk for Graves’ and a decreased risk for Hashimoto’s. But whites have the highest smoking rates in the U.S. military, which runs counter to their increased risk for Hashimoto’s and lower risk for Graves’, the study authors added.
Hennessey of Beth Israel said he suspects that genetics are a likely culprit.
“Both of these conditions are autoimmune conditions that are known to be influenced by genetic factors, and those genetic factors may be clustered more in people depending on their race,” Hennessey said.
The results of the study mirror other reports that have found elevated levels of thyroid-stimulating hormone in whites, Hennessey said. This hormone is produced by the pituitary gland and prompts the thyroid to release its own hormones into the blood.
“It sort of explains some findings we already had known, that thyroid function tests are different depending on race,” he said.
However, Hennessey noted one problem with the study that may have caused researchers to undercount cases of thyroid disease.
The researchers relied on medical coding to identify cases of either Graves’ disease or Hashimoto’s thyroiditis. However, they did not include cases more generally coded as hyperthyroidism or hypothyroidism, and there’s a chance the doctor who made the diagnosis overlooked Graves’ or Hashimoto’s as the underlying cause, he said.
More information
For more about thyroid disease, visit the U.S. Department of Health and Human Services.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










