- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
New Guidelines for Sickle Cell Disease
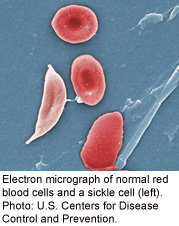
An expert panel has issued new guidelines for managing sickle cell disease, stressing the use of the drug hydroxyurea and transfusions for many with the genetic disorder.
“This is a major step forward to try to put together all of the evidence and try to highlight what is most important,” said Dr. Barbara Yawn, professor of family and community health at Olmsted Medical Center in Rochester, Minn. Yawn was also co-chair of the panel convened by the U.S. National Heart, Lung, and Blood Institute to develop the new guidelines.
As many as 100,000 Americans have sickle cell disease, according to background information with the guidelines. In sickle cell disease, the body makes sickle-shaped or crescent-shaped red blood cells. Normal red blood cells are disc-shaped, like a doughnut without holes, allowing the cells to move easily through blood vessels.
Sickle cells are stiff and sticky and tend to block blood flow, leading to organ damage, pain and increased risk of infection and strokes, among other problems. Black people are more commonly affected than other people.
The expert panel reviewed more than 12,000 scientific articles and sifted through the evidence to issue the new blueprint for care. The new guidelines are published Sept. 10 in the Journal of the American Medical Association.
One of the new recommendations is to give children oral penicillin daily until age 5. This is a preventive measure, aiming to reduce the risk of pneumonia and other infections.
“That has been the standard for a while now,” Yawn said. “Now we are saying ‘This is an absolute necessity.'”
In addition, everyone with sickle cell disease should be vaccinated against pneumonia, according to the guidelines. “The children need pneumococcal vaccine as early as they can possibly get it, around six weeks of age,” Yawn said.
Children from ages 2 to 16 should have an annual exam known as a transcranial Doppler, which measures blood flow in the brain, the guidelines explain. If it’s abnormal, long-term transfusion therapy to prevent stroke is recommended.
When acute complications occur, opioids (also known as narcotics) are suggested to treat the pain linked with blood flow blockage. A method of encouraging deep breathing — incentive spirometry — is also advised for those hospitalized with a blood flow crisis.
If adults have three or more severe blood flow crises in a year, treatment with the drug hydroxyurea is recommended. The drug works in sickle cell by helping to prevent the formation of sickle-shaped red blood cells. Hydroxyurea can be used in infants, children and teens, whether or not they currently have symptoms, according to the guidelines.
One difficulty in developing the guidelines, Yawn said, is that there is “not enough research to answer all the questions.”
People with sickle cell disease are living longer, she said. A generation ago, many with sickle cell disease only survived until their 20s or 30s. “We know there are more living into their 40s, 50s and 60s,” she said.
Dr. Michael DeBaun, professor of pediatrics and medicine at the Vanderbilt University School of Medicine, said, “These are really strong recommendations.”
DeBaun wrote an editorial to accompany the guideline report. “This should now be a road map of how your child should be cared for,” he said.
The information also applies for adults with sickle cell disease, said DeBaun, who is also director of the Vanderbilt–Meharry Sickle Cell Disease Center of Excellence.
He advises patients and parents to use the new guidelines to have a dialogue with the doctors providing care. “We expect these recommendations to change over time as more evidence becomes available,” DeBaun said.
In his own recent study, published in August in the New England Journal of Medicine, DeBaun and his colleagues reported that monthly blood transfusions appear to reduce the risk of strokes in children with sickle cell anemia, the most common form of sickle cell disease.
More information
To learn more about sickle cell disease, visit the U.S. Centers for Disease Control and Prevention.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










