- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Prescribe Blood Thinner Pradaxa With Caution, Study Warns

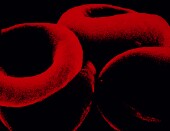
Doctors may want to use caution when prescribing the blood thinner Pradaxa for a common irregular heart beat called atrial fibrillation.
So say the authors of a new study that shows Pradaxa carries a higher risk of major bleeding and of gastrointestinal bleeding compared to the traditional blood thinner warfarin.
However, patients taking Pradaxa (dagibatran) also had a reduced risk of bleeding in the brain compared to those taking warfarin, the researchers found.
“As always, appropriate institution of any therapy requires an understanding that the ‘sword cuts both ways’ and that no potentially beneficial therapy comes without some degree of risk,” said Dr. Nicholas Skipitaris, director of cardiac electrophysiology at Lenox Hill Hospital in New York City.
“For the groups identified in this review at highest risk for bleeding on this agent, perhaps alternative therapies need to be considered,” said Skipitaris, who was not connected to the new study.
Pradaxa was approved in 2010 by the U.S. Food and Drug Administration to prevent stroke and blood clots in patients with atrial fibrillation, which has been associated with an increased risk of stroke. Since the drug’s approval, the FDA has received some reports of severe bleeding in patients taking Pradaxa.
The results, published online Nov. 3 in the journal JAMA Internal Medicine, appear to conflict with a prior U.S. Food and Drug Administration analysis of Pradaxa, one expert noted.
These findings “give us cause for concern because it appears that the bleeding risk for dabigatran is higher than for warfarin and significantly greater than originally appeared at the time of the FDA approval,” journal editor-in-chief Dr. Rita Redberg, said in an accompanying journal commentary.
“The authors note the FDA [study] failed to adjust for differences in patient characteristics, which would bias the results,” Redberg wrote. She said the new study also highlights the importance of “postmarketing” data — information regarding patient complications that is compiled after a drug has been approved.
The study was led by Inmaculada Hernandez of the University of Pittsburgh and included more than 9,400 Medicare patients diagnosed with atrial fibrillation in 2010 and 2011. About 1,300 were prescribed Pradaxa and more than 8,100 received warfarin.
All of the patients were followed until they either stopped using the drugs, switched to a different blood thinner, died or until December 2011.
“To the best of our knowledge, our study is the first to compare the safety profile of dabigatran and warfarin using a nationally representative sample of Medicare beneficiaries,” the researchers wrote in the news release.
The study showed rates of major bleeding were 9 percent for those taking Pradaxa and nearly 6 percent for those taking warfarin. The risk of major bleeding was especially high among black patients and those with chronic kidney disease, Hernandez’ team found.
Patients taking Pradaxa were also more likely to have gastrointestinal bleeding. On the other hand, those taking warfarin had a higher risk for intracranial (brain) bleeding, according to the study.
According to Skipitaris, “the risk of intracranial bleeding — arguably more serious than GI bleeding — is less on Pradaxa compared to warfarin, so this agent is still clinically useful.”
More information
The U.S. Agency for Healthcare Research and Quality has more about blood thinners.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










