- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
‘Hidden’ Brain Damage Seen in Vets With Blast Injuries: Study

The brains of some veterans of Iraq and Afghanistan who were injured by homemade bombs show an unusual pattern of damage, a small study finds.
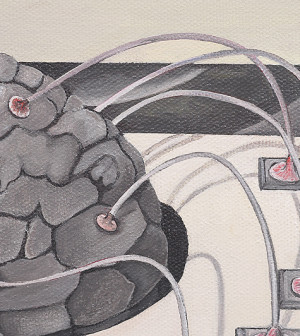
Researchers speculate that the damage — what they call a “honeycomb” pattern of broken and swollen nerve fibers — might help explain the phenomenon of “shell shock.”
That term was coined during World War I, when trench warfare exposed troops to constant bombardment with exploding shells. Many soldiers developed an array of symptoms, from problems with vision and hearing, to headaches and tremors, to confusion, anxiety and nightmares.
Now referred to as blast neurotrauma, the injuries have become an important issue again, said Dr. Vassilis Koliatsos, the senior researcher on the new study.
“Vets coming back from Iraq and Afghanistan have been exposed to a variety of situations, including blasts from improvised explosive devices [IEDs],” said Koliatsos, a professor of pathology, neurology and psychiatry at Johns Hopkins University in Baltimore.
But even though the recognition of shell shock goes back 100 years, researchers still know little about what is actually going on in the brain, Koliatsos said.
For the new study, published recently in the journal Acta Neuropathologica Communications, his team studied autopsied brain tissue from five U.S. combat veterans.
The soldiers had all survived IED bomb blasts, but later died of other causes. The researchers compared the vets’ brain tissue to autopsies of 24 people who had died of various causes, including traffic accidents and drug overdoses.
According to Koliatsos, the soldiers’ brains showed a distinct pattern of damage to nerve fibers in key regions of the brain — including the frontal lobes, which govern memory, reasoning and decision-making.
He said the “honeycomb” pattern of small lesions was unlike the damage seen in people who died from head trauma in a car accident, or those who suffered “punch-drunk syndrome” — brain degeneration caused by repeated concussions.
According to Koliatsos, before their deaths the five vets did show signs of “neuropsychiatric” problems, such as depression and anxiety. One died of a gunshot wound to the head, and three died of methadone overdose. Those overdoses could have been accidental, since the drug is prescribed for severe pain, he noted.
It’s not clear whether any of the soldiers’ symptoms can be blamed on the brain damage seen in this study, according to Koliatsos.
But, he said, “you have to raise the question, ‘Could the neuropsychiatric problems be related to this frontal lobe dysfunction?'”
Another expert said it “provides preliminary evidence to support structural and physical changes associated with blast [brain] injuries.”
“I think this is an important next step in our understanding of how blast injuries can impact military personnel and veterans, even if we can’t easily ‘see’ the injuries using traditional medical techniques,” said Craig Bryan, executive director of the National Center for Veterans Studies at the University of Utah, in Salt Lake City.
Both he and Koliatsos said further studies are needed to confirm these findings, and to understand what this brain damage “signature” means.
“My hope is that research such as this will eventually lead to better diagnostic tests that can detect and identify otherwise hidden injuries much sooner,” Bryan said.
It could also lead to more refined treatment, according to Koliatsos. For example, if damage to the frontal lobes is causing some blast-injured veterans’ symptoms, then treatment might include medications that stimulate the frontal lobes.
But that’s for future studies to figure out. “It’s premature to say what this means for veterans right now,” Koliatsos said.
The most important thing, he added, is for blast-exposed vets to seek treatment for any lingering symptoms.
“If you’re having problems, talk to your family and talk to your doctor,” Koliatsos said.
More information
The Defense and Veterans Brain Injury Center has more on traumatic brain injuries.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










