- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
Gene Testing May Boost Lung Cancer Survival: Study

WEDNESDAY, Oct. 30Chances of surviving lung cancer longer increase when treatment is personalized based on the genetics of the cancer, German researchers report.
Knowing the tumor’s genetic signature can help doctors spot differences in cancer cells that may lead to a more accurate diagnosis and better-targeted therapy, the researchers explained.
“Gene classification and diagnosis has a profound impact on patients’ survival,” said study co-author Dr. Reinhard Buttner, a professor of pathology at University Hospital Cologne.
“Our data were collected from approximately 5,100 lung cancer patients and show that genotyping of lung cancer doubles overall survival in patients with two specific mutations — EGFR-mutated and ALK-translocated,” Buttner said.
Patients with those mutations who received personalized therapies showed survival advantages ranging somewhere between 12 months and 21 months.
The report was published Oct. 30 in the journal Science Translational Medicine.
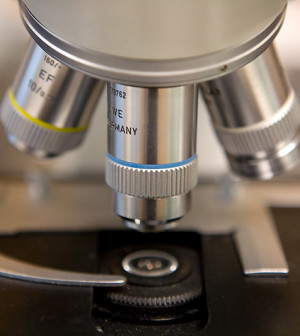
The researchers found that although some lung cancer cells look the same under the microscope, they may actually be quite different genetically.
“Systematic profiling of gene mutations in lung cancer allows precise classification and diagnostics and predicts the efficacy of targeted and personalized therapies. Every lung cancer should be analyzed for mutations to find the best therapy,” Buttner said.
Surprisingly, looking at two common types of lung cancer — small-cell and large-cell — from a genetic perspective actually ended up eliminating large-cell lung cancer as a distinct category, he said.
In addition, genotyping identifies many cancer mutations that might be targeted with therapies in new clinical trials, Buttner said.
The bottom line is that knowing the genetics of a cancer can help personalize treatment and improve survival. “Gene characterization of lung cancers and probably other cancers allows selective therapies, which immediately improve survival,” he said.
“This analysis of tumors in lung cancer, at the end of the day, leads to a better prognosis,” said study co-author Dr. Thomas Zander, a research fellow in the lung cancer group at University Hospital Cologne. “That’s because a patient can get a personalized treatment.”
“I am convinced that this will be the future of cancer treatment, not only for lung cancer, but for nearly every type of cancer,” Zander said.
A U.S expert not involved with the study agreed about the importance of genetic analysis and personalized treatment.
“Genetic analysis is going to become an intrinsic part of cancer treatment. There is a lot of promise that this is the best way of treating patients going forward,” said William Phelps, scientific program director at the American Cancer Society.
The other part of personalized treatment is the development of new drugs that target particular gene mutations, Phelps said.
“There are limited drugs available now. You are going to see more drugs available, so genetic testing will be that much more valuable going forward as more targeted therapies become available,” he said.
Phelps noted that such analysis is being performed, but on a limited scale. “Not everyone has the capability to do this. You not only have to be able to do the genetic analysis, but you also have to be able to tell which mutations are meaningful and which ones are not,” he said.
But the process is starting and being tested at the major cancer centers, Phelps added. “I think this is where we are evolving to. It’s not widely available yet, but we are trying to make it more widely available,” he said.
As in the United States, access to gene typing of cancer in Germany is limited to major cancer centers. “One of the things we want to do is increase the visibility of gene typing so that more patients and more doctors are aware of it,” study co-author Zander said.
More information
For more about lung cancer, visit the American Cancer Society.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










