- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
Most Cases of Dementia in U.S. Seniors Go Undiagnosed: Study
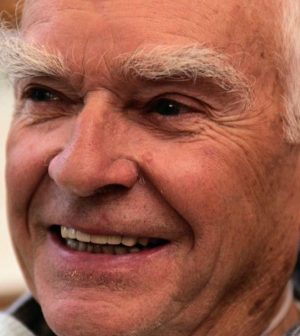
Most Americans with dementia are undiagnosed, which shows how important it is to screen and assess seniors for the disease, researchers say.
Their new analysis of data from a nationwide survey of about 6 million Americans aged 65 and older revealed that 91% of people with cognitive impairment consistent with dementia did not have a formal medical diagnosis of dementia or Alzheimer’s disease.
When other people (generally, family members) responded to the survey, the rate fell to around 75%, which is still significant, said study co-author Sheria Robinson-Lane. She is a gerontologist at the University of Michigan School of Nursing, in Ann Arbor.
Rates of non-diagnosis varied by race, gender and education. For example, Black seniors had a higher rate (93%) than other racial groups, according to the report published June 29 in the Journal of Alzheimer’s Disease.
“There is a large disparity in dementia-related treatment and diagnosis among Black older adults, who are often diagnosed much later in the disease trajectory compared to other racial and ethnic groups,” Robinson-Lane said in a university news release.
Men (99.7%) were more likely to report no diagnosis than women (90.2%), and those who didn’t graduate high school had a higher estimated rate (93.5%) than those with at least a high school education (91%), the findings showed.
Higher education is often associated with greater wealth and more access to resources that affect both dementia risk and disease progression, Robinson-Lane noted.
There’s also evidence that education level may affect results on thinking and memory (“cognitive”) tests.
Robinson-Lane said the findings are particularly relevant now because people with dementia have higher risk for COVID-19 hospitalization and death. COVID-19 also causes long-lasting neurological impacts in some people, perhaps increasing their dementia risk.
Dementia screening isn’t a routine part of annual well visits for older adults, she noted.
“Now more than ever, these routine screenings and assessments are really critical,” Robinson-Lane said. “I think it’s particularly important to have some baseline information available to providers of patients over 65.”
Co-author Ryan McGrath, an assistant professor of health, nutrition and exercise sciences at North Dakota State University in Fargo, said evaluating seniors’ thinking skills is important.
“We recommend that health care providers screen for low cognitive functioning during routine health assessments when possible,” McGrath said. “A telemedicine option may reduce clinic time and expand reach.”
More information
The U.S. National Institute on Aging has more about dementia.
SOURCE: University of Michigan, news release, June 23, 2021
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










