- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
‘Silent’ Seizures Tied to Alzheimer’s Symptoms
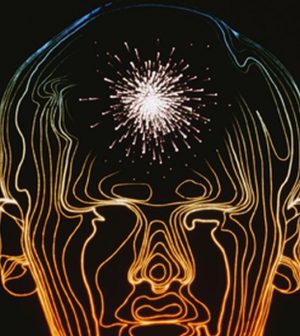
Undetected or “silent” seizures may contribute to some symptoms associated with Alzheimer’s disease, such as confusion, a small study suggests.
The seizures occur in the hippocampus — a part of the brain involved in the consolidation of memories. Researchers suspect that treating these seizures could help manage Alzheimer’s or possibly slow it down.
“While it is not surprising to find dysfunction in brain networks in Alzheimer’s disease, our novel finding that networks involved in memory function can become silently epileptic could lead to opportunities to target that dysfunction with new or existing drugs to reduce symptoms or potentially alter the course of the disease,” said study senior author Dr. Andrew Cole.
Cole directs the Massachusetts General Hospital (MGH) Epilepsy Service.
“We now have to study more individuals to validate this finding and understand how prevalent it is in Alzheimer’s patients, whether it occurs in other neurodegenerative disorders and how it responds to treatment,” he said in a hospital news release.
The study involved only two women. They were both in their 60s with symptoms associated with Alzheimer’s disease. The women had bouts of confusion or asked the same questions repeatedly.
Brain images and cerebrospinal fluid tests suggested they had Alzheimer’s, but swings in the women’s symptoms were much more dramatic than usual.
Neither of the women had a history of seizures. Normally, a test called an EEG conducted from the scalp can detect abnormal electrical activity in the brain of people who have seizures. But, in these two women, no such abnormalities were found, the researchers said.
Since the hippocampus is a key part of the brain affected by Alzheimer’s disease, and also a common source of seizures in people with epilepsy, the researchers honed in on that part of the brain and conducted additional tests.
Electrodes were placed on both sides of the women’s brains through a naturally occurring opening at the base of the skull. Their brain activity was monitored for 24 to 72 hours.
The study found the women had seizure-like activity in the hippocampus. One woman had frequent surges of electrical activity usually associated with seizures that were not picked up by the scalp EEG. Three seizures occurred during sleep. None of these episodes caused any noticeable symptoms.
Anti-seizure drugs eliminated the seizure-like activity. In the year that followed, the woman only had one incident of confusion, which occurred when she missed doses of her medicine.
The other woman also had frequent spikes in electrical activity in the hippocampus during sleep. This patient was also treated with anti-seizure medication but the treatment was discontinued due to unwanted mood-related side effects.
“Our findings confirmed the presence of serious dysfunction of the neuronal networks affected by Alzheimer’s disease and confirmed our hypothesis that epileptic phenomena are an important component of that disturbance,” said Cole.
But, he added, more study is needed. The researchers hope to develop a way to detect these silent seizures without using the minimally invasive electrodes in the brain.
The study was published online May 1 in Nature Medicine.
More information
The U.S. National Institute on Aging provides more information on Alzheimer’s disease.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










