- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Many Breast Cancer Patients Get Too Much Radiation Therapy, Research Suggests

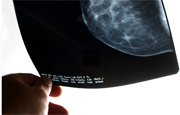
WEDNESDAY, Dec. 10, 2014 (HealthDay News) — Many studies have affirmed that a newer, shorter course of radiation therapy for early-stage breast cancer works just as well as a longer course.
However, new research suggests that many U.S. patients still get radiation therapy for much longer than they need to.
The analysis of data, involving millions of women, found that two-thirds of breast cancer patients who’ve had breast-conserving surgery (lumpectomy) undergo six to seven weeks of radiation therapy.
However, multiple studies suggest that an alternative course of only three weeks of higher-dose radiation — called hypofractionated whole breast radiation — is just as effective, more convenient and cheaper than longer, conventional radiation therapy, according to the study authors.
The newer type of radiation therapy is supported by four studies and practice guidelines from the American Society for Radiation Oncology, the researchers noted.
The study was published in the Dec. 10 issue of the Journal of the American Medical Association.
One expert wasn’t surprised by the finding.
The reasons behind the continued overuse of the longer course of radiation treatment “need to be investigated to further elucidate why there has been a slow transition to the shorter course of therapy,” said Dr. Stephanie Bernik, chief of surgical oncology at Lenox Hill Hospital in New York City.
“In the meantime, women need to raise the issue with their radiation oncologist to see if they qualify for the three-week course of radiation,” she said.
The study found that in 2013, only 34.5 percent of early-stage breast cancer patients older than 50 received the shorter-course hypofractionated therapy. That’s at least a higher percentage than the roughly 11 percent of women who were using the newer radiation regimen in 2008, said researchers led by Dr. Justin Bekelman, an assistant professor of radiation oncology, medical ethics and health policy at the University of Pennsylvania.
Among younger women and those with more advanced cancers, about 21 percent received hypofractionated therapy in 2013, compared with about 8 percent in 2008, the study also found.
However, use of the newer, shorter-course therapy has accelerated much more in Canada, the study found. In that country, more than 70 percent of early-stage breast cancer patients were already receiving hypofractionated radiation therapy by 2008, Bekelman’s team found.
There were cost issues, too. The study found that the use of hypofractionated radiation therapy reduced insurers’ costs in the first year after breast cancer diagnosis by 10 percent.
The switch to the shorter-course therapy had little effect on patients’ out-of-pocket costs, the researchers found, but it did reduce the time patients needed to be away from work and home, which means they did get economic and quality-of-life benefits.
Still, in the United States, the shorter course of radiation is still “infrequently used for women with early-stage breast cancer, even though it’s high-quality, patient-centric cancer care at lower cost,” Bekelman said in a university news release.
“It is clinically equivalent to longer duration radiation in curing breast cancer, has similar side effects, is more convenient for patients, and allows patients to return to work or home sooner,” he added.
Another expert agreed, but said more research is needed to determine which types of patients will benefit most from shorter-course therapy.
“Shorter-course treatment offers a significant advantage to these patients in terms of convenience and cost with a similar side effect profile to conventional breast treatment,” said Dr. Sheryl Green, an assistant professor of radiation oncology at the Icahn School of Medicine at Mount Sinai in New York City.
“However, additional studies are still needed to fully evaluate both the effectiveness and safety of such treatment in particular subgroups, such as very young women, women with large breasts and/or more advanced tumors and positive nodes,” Green added.
“Further data also needs to be obtained to evaluate the tolerability and safety of shorter radiation treatment scheduled when used in conjunction with other therapies,” she said.
In the meantime, Green said, “we recommend that women discuss these options with their radiation oncologist to determine the optimal treatment regimen for their particular case.”
More information
The U.S. National Cancer Institute has more about breast cancer treatment.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










