- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
- How Daily Prunes Can Influence Cholesterol and Inflammation
Deep Brain Stimulation Therapy May Help Parkinson’s Patients Long Term
Parkinson’s disease patients can get symptom relief with deep brain stimulation (DBS) therapy that lasts over the long term, a new study shows.
Over 15 years, patients who received DBS, which requires surgical implantation, had significant improvement in motor symptoms and less need for medication, researchers found.
“Our study, for the first time, supports the efficacy of deep brain stimulation in the very long term — 15 years after surgery and 25 years since Parkinson’s diagnosis,” said senior researcher Dr. Elena Moro, director of the Movement Disorders Unit at Grenoble Alpes University in France.
“Indeed, after an average of 15 years after surgery, patients could experience improvement, compared to before surgery,” she said. “Moreover, we could still observe a marked reduction of anti-Parkinson’s medication and improvement of quality of life, compared with before the intervention.”
Patients with Parkinson’s disease no longer make dopamine, which affects their speech, walking and balance. Symptoms can be partially relieved by the drug levodopa, which temporarily restores dopamine.
But as levels of dopamine fluctuate during the day, patients can suffer from dyskinesia, a side effect of levodopa that can cause twisting, swaying or head bobbing.
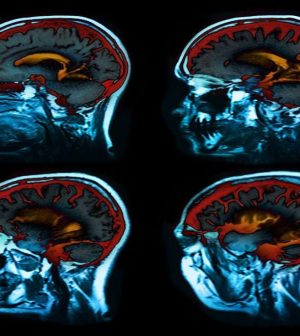
Deep brain stimulation uses electrodes placed in areas of the brain to control Parkinson’s symptoms. The electrodes connect to a pacemaker-like device placed under the skin in the upper chest that transmits an electrical pulse that helps to control symptoms. Many patients use a handheld controller to adjust stimulation levels as needed.
For the study, Moro’s team collected data on 51 patients being treated with DBS. On average, they had the device for 17 years.
Compared with data from before the implant to that after 15 years, the number of times patients experienced dyskinesia was cut by 75%. Use of medications to control dopamine levels was reduced by 51%, and the amount of time when medication was no longer working well dropped 59%.
Researchers found few side effects from having the device for 15 years, and those were mostly manageable.
DBS is recommended for advanced Parkinson’s, and Moro said surgery should not be delayed when motor conditions and quality of life decline despite other treatment.
“This information is relevant for physicians, patients and their families when they need to decide about the surgical option to deal with Parkinson’s,” she said. “People with Parkinson’s should know that the beneficial effects of deep brain stimulation surgery will last beyond 15 years.”
Dr. Michael Okun, national medical adviser to the Parkinson’s Foundation, said DBS, when used with medications, has long-lasting effects in some patients. He was not part of the study.
“These long-term studies tell us a number of things,” said Okun, who is chairman and professor of neurology at the University of Florida. “The most important thing they tell us is that disease continues to progress despite the intervention.”
Neither deep brain stimulation nor medication is a treatment for the disease itself. “Where you do get benefits long-term are things like dyskinesias and motor fluctuations,” Okun said.
Patients who do well on levodopa are most likely to benefit from DBS, he said.
Patients who are still benefiting from the device after 15 years are those whose disease is progressing slowly. People whose Parkinson’s progresses more quickly aren’t around to be evaluated after 15 years, Okun said.
“We have people in our practices who have had Parkinson’s for 30 years or more,” he said. “The real lesson of deep brain stimulation is to choose the folks who have a good response to levodopa before you implant.”
DBS is not good for walking, talking, thinking and balance, Okun said.
“In the long term, it does help in smoothing out fluctuations, suppressing tremors and shaking,” he said. “It’s hopeful for features that still respond to dopamine, so if your rigidity or stiffness still responds to dopamine, it’s going to be helpful. That’s where it has its biggest bang 15 years down the road.”
Okun stressed again that Parkinson’s progresses no matter how it is treated.
“What we found in the deep brain stimulation populations is they still are prone to get dementia, so they’re still just like regular Parkinson disease folks, they still get walking, talking and thinking problems, and those things are not treated well by this hardware solution,” Okun said.
The findings were published online June 2 in the journal Neurology.
More information
To learn more about Parkinson’s disease treatment, visit the Parkinson’s Foundation.
SOURCES: Elena Moro, MD, PhD, director, Movement Disorders Unit, Grenoble Alpes University, Grenoble, France; Michael Okun, MD, national medical adviser, Parkinson’s Foundation, and chairman and professor, neurology, University of Florida, Gainesville; Neurology, June 2, 2021, online
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










