- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
Infant’s Early Diet Doesn’t Change Celiac Disease Risk, Study Finds

A newborn’s risk of developing celiac disease isn’t reduced by breast-feeding. Nor will delaying the introduction of a protein found in wheat called gluten to an infant’s diet help prevent celiac disease.
Those are the conclusions from a pair of new studies in the Oct. 2 New England Journal of Medicine.
The new findings put to rest hopes that a child could avoid celiac disease if mothers breast-feed their babies and introduce gluten between 4 and 6 months old, said Dr. Alessio Fasano, co-author of one of the studies and director of the Center for Celiac Research and Treatment at MassGeneral Hospital for Children.
“Contrary to our strong belief, breast-feeding does not help to prevent celiac disease at all,” Fasano said. “We’re not saying breast-feeding is useless. It can definitely have benefits for other reasons, but not for preventing celiac disease.”
Instead, it appeared to researchers that celiac disease is influenced solely by genetics. Inheriting a genetic predisposition to autoimmune disorders proved the only way that researchers could predict a baby’s future risk of celiac disease.
“We know some of the genes you must have to develop celiac disease, and if you have two copies of the gene, the risk of developing celiac disease increases dramatically,” Fasano said.
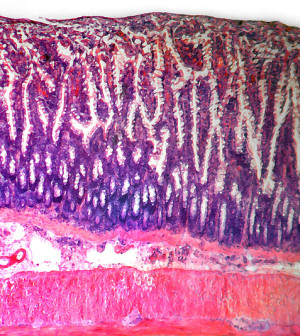
Celiac disease is a disorder in which the immune system attacks and damages the small intestine. These attacks are prompted by the consumption of gluten, a protein found in wheat and other related grains, which can promote a vicious immune system response in some people, according to the Celiac Disease Foundation.
Previous research had indicated that breast-feeding might have a protective effect against celiac disease in babies, researchers noted in background information in the study. Other studies had indicated there could be a window between 4 and 6 months during which a child exposed to gluten might be more likely to build up a tolerance.
The first study involved more than 700 Italian infants enrolled between 2003 and 2008, and thought to be at risk because a member of their immediate family had celiac disease.
The children were randomly assigned to two groups, one in which children began eating foods with gluten at 6 months and another where they waited until their first birthday before eating gluten. Researchers then followed the children for five years.
Postponing the introduction of gluten had no effect on a child’s long-term risk of developing celiac disease, the study found.
However, it did delay the onset of celiac disease, which could prove vital in protecting a child’s healthy development, Fasano said.
“A delay of 8 to 10 months can be important,” he said. “This time is crucial for the development of many organs, including the brain.” The immune response associated with celiac disease could be detrimental to normal development, so delaying it as long as possible might be worthwhile, according to the study authors.
Breast-feeding did not affect the development of celiac disease either way, the researchers also noted.
The study also found that children who had certain genes that influence the human leukocyte antigen (HLA) system were twice as likely to develop celiac disease than children with normal-risk HLA genes. HLA helps direct the immune system to attack specific targets, and if faulty can lead to autoimmune disorders.
The second study involved more than 900 children also at high risk for celiac disease, about half of whom received gluten in their daily diet from 16 weeks to 24 weeks of age. This study also concluded that the introduction of small quantities of gluten did not reduce risk of celiac disease.
Dr. Ivor Hill, a pediatric gastroenterologist at Nationwide Children’s Hospital in Columbus, Ohio, said he was not surprised by the results of the two studies.
“It has always been my belief the idea that we could prevent celiac disease in infants through diet would not hold up,” he said. “We were delaying the age of onset, but we could not prevent it.”
Hill said parents would best be served by monitoring children in families with a predisposition to celiac disease. “There’s not a lot you can do outside staying away from gluten for the rest of your life,” he said.
HLA testing of these children would help determine a child’s future risk, but “at this time, that’s not a cheap test. That’s a very expensive test,” Hill said, adding that newer techniques are being investigated that could bring the price down.
The findings from these studies don’t address people who have non-celiac gluten sensitivity, according to the authors of an accompanying editorial in the same issue of the journal. A gluten sensitivity produces symptoms similar to celiac disease, but no damage occurs to the small intestine from consuming gluten, according to the Celiac Disease Foundation.
More information
For more information on celiac disease, visit the National Institutes of Health.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










