- Comparing Whey and Plant-Based Protein: Which is Best?
- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
Better Control of Drug-Resistant Germs Could Save Thousands of Lives: CDC

An immediate, focused effort to halt the spread of antibiotic-resistant germs could save tens of thousands of lives and prevent hundreds of thousands of new infections over the next five years, a new government report suggests.
As many as 37,000 lives could be saved, and 619,000 new infections prevented, if community health departments and health care facilities form tight support networks to quickly identify and address emerging outbreaks of antibiotic-resistant bacteria, said report author Dr. John Jernigan.
He directs the Office of HAI (Health care-Associated Infections) Prevention Research and Evaluation at the U.S. Centers for Disease Control and Prevention.
“When health care facilities and health departments in a community work together to share information about resistance, and then use that information to guide and target prevention efforts, then we would expect to see up to 70 percent fewer patients affected by drug-resistant germs,” Jernigan explained.
Although local health departments will probably need increased funding to coordinate these efforts, the CDC report estimates that almost $8 billion in hospital bills could be avoided over five years by halting the spread of antibiotic-resistant bacteria.
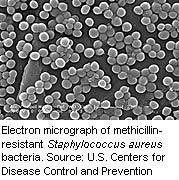
Antibiotic-resistant germs like methicillin-resistant Staphylococcus aureus(MRSA) and CRE, which no longer respond to drugs designed to kill them, cause more than 2 million illnesses and at least 23,000 deaths each year in the United States, according to the CDC.
The powerful antibiotics needed to treat these germs also leave patients vulnerable to Clostridium difficile, an opportunistic bacteria that invades a person’s gut after antibiotics have wiped out the intestinal flora that normally would fend off such an infection.
C. difficile caused close to a half-million illnesses in 2011, and an estimated 15,000 deaths a year are directly attributable to the life-threatening diarrhea that results from C. difficile infections, the CDC added.
Computer models show that these bugs will continue to gnaw away at America’s health care system, according to the Vital Signs report published Aug. 4 in the CDC’s Morbidity and Mortality Weekly Report.
“Over the next five years, unless we implement nationwide improvements in infection control and antibiotic prescribing, if no action is taken, these infections will continue to increase,” Jernigan said.
Individual hospitals are trying to control the spread of antibiotic-resistant germs, but those efforts are being undermined by other hospitals and long-term care facilities, the CDC researchers found.
“We know that germs can spread between health care facilities in a community, when patients are transferred from one facility to the other,” Jernigan explained. “Antimicrobial resistance problems in one hospital can affect what happens in another hospital when they share patients. Even if one facility is following recommended infection control practices, that doesn’t protect them from patients bringing antimicrobial-resistant germs into their facility from other hospitals or nursing homes.”
Jernigan said community health departments are in the perfect position to coordinate infection control between hospitals, since they already are collecting information on health care-associated infections and antibiotic resistance.
If a health department detects a problem at a hospital, it can notify that hospital and all other facilities connected with it that infection control efforts need to be stepped up, he said. Patients carrying resistant bugs can be placed in private rooms, health care workers can take additional precautions to prevent the spread of germs, and more caution can be used with antibiotics.
But Jernigan said nursing homes and other long-term care facilities need to be brought into the network, since many patients bring antibiotic-resistant germs with them when they are transferred to hospitals.
Dr. Eric Howell, immediate past president of the Society of Hospital Medicine, agreed that long-term care facilities are key members of a community’s network and need to be included in efforts to track infections.
“It really needs to include all of the health care institutions. The trick is to make it so people want to participate because it’s valuable to them,” said Howell, division director of the Collaborative Inpatient Medicine Service at Johns Hopkins Bayview Medical Center in Baltimore. “People participate not because it’s mandated, but because it’s a high-value data repository for the hospital and their individual clinicians. They’re willing to input data because they get so much out in return.”
The CDC has included $264 million in its budget for the 2016 fiscal year to strengthen surveillance efforts and promote better collaboration among health care facilities, Jernigan said. The agency’s Antibiotic Resistance Solutions Initiative is expected to reduce infections of CRE, MRSA and C. difficile by half or more if successfully implemented, officials said.
However, federal laws that protect patient privacy could be an obstacle, since they hamper the ability of hospitals to share information, said Dr. Henry Chambers, chief of the division of infectious diseases at San Francisco General Hospital and a professor at the University of California, San Francisco, School of Medicine.
“I think the laws are over-interpreted and actually interfere with a number of health care measures,” Chambers said. “You’ve got to know who’s who, right? If you’re one of those people who has an antibiotic-resistant infection, there has to be a way to communicate that at an institutional level and not a provider level.”
More information
Visit the U.S. Centers for Disease Control and Prevention for more on antibiotic resistance.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










