- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
Hospitals’ High Antibiotic Use May Boost Germs’ Resistance: Study
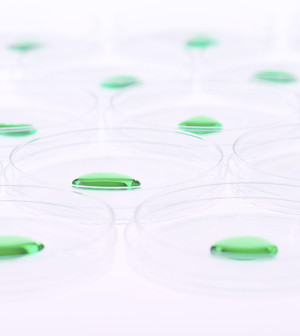
About half of all U.S. hospital patients receive antibiotics, and these drugs are commonly the ones more likely to promote the growth of antibiotic-resistant bacteria, a new study found.
“This is where the bad bugs spread, in the hospitals, because so many people are receiving antibiotics, and one of the only things that can spread are the antibiotic-resistant bugs,” said Dr. Eli Perencevich, an infectious disease epidemiologist at the University of Iowa Carver College of Medicine.
“We have to figure out better ways to reduce excess antibiotic use, and one way to do that is to get better at making diagnoses,” he added.
The study identified how many of more than 11,000 patients received antibiotics on a given day at one of 183 hospitals throughout the United States in 2011. The researchers found that 50 percent of these patients got at least one antibiotic, and about half of those patients received two or more antibiotics.
The study, led by researchers at the U.S. Centers for Disease Control and Prevention, was published in the Oct. 7 issue of the Journal of the American Medical Association. The CDC also funded the study.
The most common reasons for the antibiotics were lower respiratory tract infections, followed by urinary tract infections and skin or soft tissue infections. About 76 percent of the patients received antibiotics to treat infections, and about 19 percent received them to reduce the risk of infection during surgeries, the study found.
More problematic, however, was that the most commonly used medications were broad-spectrum antibiotics, likely due to “fear of targeting the wrong pathogen or missing a resistant organism, especially in a sick patient,” said Dr. Mary Anne Jackson, director of infectious diseases at Children’s Mercy Hospital and Clinics in Kansas City, Mo.
“There are good bacteria, such as on our skin and in our mouth and intestine, that are normal and vital to keeping us healthy,” Jackson said. An infection, on the other hand, is caused by pathogens, the “bad” bacteria. While narrow-spectrum antibiotics primarily target specific germs — mostly the harmful ones — broad-spectrum antibiotics go after a broader range of bacteria, which can kill helpful bacteria as well.
It’s the broad-spectrum antibiotics, Perencevich added, that are thought to increase the risk of a patient developing an infection caused by bacteria that is resistant to most antibiotics.
“In general, it’s better to have someone on a narrow-spectrum antibiotic that treats the specific bacteria causing the infection,” he said. But that is difficult to do, he added, if doctors are unsure what is causing a patient’s infection or other symptoms.
Dr. Shelley Magill, of the CDC’s Division of Healthcare Quality Promotion, was particularly concerned to see that broad-spectrum drugs and drugs that treat resistant bacteria were often used for patients outside of intensive care units and for community-onset infections — not the most critically ill patients.
“Antimicrobial drugs are truly precious resources that have saved so many lives over the years. We need to use them judiciously if we are to preserve their effectiveness for future generations,” Magill said.
When it’s not clear exactly what type of pathogen is causing the infection and the patient’s condition is serious, “broad-spectrum antimicrobial drug use is often appropriate and critically important,” Magill said.
But once test results are available, Magill said it’s important to take an “antibiotic time-out” to determine whether to switch to a narrow-spectrum drug or to stop drugs altogether.
While overuse of antibiotics due to patient demand can occur frequently in the outpatient setting, such as at the pediatrician’s office, Perencevich and Jackson said it is less likely that it is occurring in the hospital.
“Doctors lean on antibiotics because even if there’s a small chance they’ll work, that’s worth it when you have a sick patient,” Perencevich said. “Until we have better diagnostic tests, it will be harder to control antibiotic use in hospitals.”
There was a silver lining in the study, Perencevich said.
“The encouraging thing was that most of the antibiotics were given for a specific reason, and only 7 percent had no rationale listed,” he said.
The two keys to reducing broad-spectrum antibiotic use further, he said, are improved diagnostics and the implementation of systems that track antibiotic use in real time so that doctors can learn how to improve antibiotic use.
More information
The U.S. Centers for Disease Control and Prevention has more about antibiotic resistance.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










