- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
Modern War Wounds Can Devastate Vets’ Sexual, Emotional Health

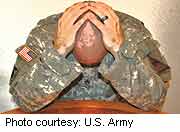
The tools of war have changed. With the increased use of powerful explosive devices, men and women patrolling on foot in bomb-laced areas of combat are increasingly suffering traumatic injuries to the groin and genitals, experts say.
Those injuries can pose complex long-term sexual and psychological challenges.
It is hard to even imagine having your genitals crushed, burned or ripped off in a blast by a makeshift bomb, said Dr. Chris Gonzalez, the lead author of a new review article published recently in The Journal of Men’s Health. “For some, it’s even worse than losing a limb,” he said.
The impact of so-called “improvised explosive devices” (IEDs) is different from gun fire encountered in earlier combat, explained Gonzalez, who is a professor of urology at Northwestern University Feinberg School of Medicine, in Chicago.
“The energy comes from the ground up, so the first thing that gets hit is in the perineal [groin] area,” he said.
The rising use of IEDs by enemies in countries like Iraq and Afghanistan has led to a more than three-fold rise in the rate of genital and urinary injuries to men and women in combat, according to Gonzalez. In fact, IEDs are now the leading cause of all combat-related casualties, accounting for about two-thirds of genital-urinary injuries. These types of wounds can affect the penis, testicles, bladder, urethra, vagina, ovaries, intestines, and rectum, Gonzalez said.
Surgeries and subsequent problems and complications can often string out over months, requiring a wide range of health providers, support and help navigating the health care system, Gonzalez added. Blast-caused problems often include post-traumatic stress disorder and other serious psychological issues associated with the loss of sexual function and fertility, he said.
Too often, these issues are not managed effectively by the health care system, Gonzalez believes. “The VA [Veterans Administration] has done a great job in dealing with limb loss and traumatic brain injuries, but with these injuries, the care can be fragmented,” he said.
Patients also experience problems that impair their relationships — issues with intimacy, parenting and self-worth, Dr. Janice Bray, chief of Central Texas Veterans Health Care System, said in an editorial accompanying the review article. Veterans with these type of groin injuries often have an increased suicide risk, she said.
Silence is a big contributor. “People are uncomfortable talking about these issues,” said Bray. “There’s a shyness about it. There’s not an open dialog, and there’s a taboo about these parts of our body.”
As a result, Bray said patients don’t want to broach the topic of sexual function or relationship problems associated with their injuries; they assume physicians would bring up the issues if they thought they were important. And doctors too often believe that if something were bothering patients, the patients would ask questions.
The sheer scope of these wounds demands new, coordinated approaches to care, Gonzalez believes.
He said medical disciplines have long been run in isolation, with inadequate communication between various specialties. “We’re so super-specialized now and medicine has moved away from coordinated care,” he said.
To help these patients, health care providers need to identify the broad range of problems these patients have, and work collaboratively to address them, he added.
But Bray, a psychiatrist, said it’s going to be difficult to get physicians from different specialties to talk with each other. For example, “I have no interaction with surgeons,” she said. “Communication is on paper or electronic, and you communicate without having a discussion. There’s not a lot of time built in to interact and work together.”
Isn’t there some way to prevent these wounds in the first place? It’s tough, said Gonzalez. While there are several types of body armor designed to help reduce the impact of IEDs, they typically are not designed for the groin and are not widely used, he explained.
As for fertility issues, some men and women who are deployed to high-risk areas may have sperm taken and preserved before deployment, just in case, said Gonzalez. There are also ways to extract and preserve sperm after an injury has occurred, he added.
There may be some good news, however. In December, President Obama signed the National Defense Authorization Act — legislation that contained an amendment that requires the Department of Defense and the Department of Veterans Affairs to create a comprehensive policy for treating service members with wounds to their urinary-genital areas. Urological associations worked to advance the issue of treating in Congress and to get the amendment into the Act, Gonzalez said.
“This bill will look at the research, prevention including better body armor and what’s the best way to manage these folks at the battlefield, stateside, and in rehabilitation,” Gonzalez explained.
More information
Learn more about explosions and blast injuries from the U.S. Centers for Disease Control and Prevention.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










