- Comparing Whey and Plant-Based Protein: Which is Best?
- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
Common MS Meds Might Be Less Effective in Black Patients
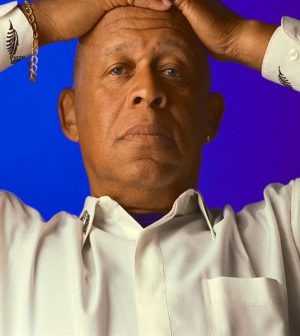
Black people experience more severe courses of multiple sclerosis (MS), and now new research suggests that drugs commonly used to treat this disease may not work as well or for as long in these folks.
“I was amazed,” said study researcher Dr. Gregg Silverman, a professor of medicine at NYU Langone Health in New York City. In a study of two drugs, “there was a dramatic and significant difference between responses of Black and white participants.”
MS occurs when your body’s immune system engages in friendly fire against your brain, spinal cord and optic nerves or central nervous system. This damages the myelin, a fatty substance that surrounds and insulates the nerve fibers. Symptoms may include difficulty walking, numbness, tingling, weakness and/or vision problems, according to the National MS Society.
There is no cure for MS, but today’s treatments can help relieve symptoms and prevent the disease from progressing.
The new study included 134 people with MS and 32 with a similar disease called neuromyelitis optica spectrum disorder. Participants received infusions of rituximab or ocrelizumab. Both drugs destroy B-cells in the blood. Ocrelizumab (Ocrevus) is U.S. Food and Drug Administration-approved to treat MS, but rituximab (Rituxan) is not.
The group included 61 Black people and 60 white people. Black and white folks showed no difference in the levels of B-cells in their blood four to six months after their infusions, but when researchers looked at B-cell levels up to 12 months post-infusion, 76% of the Black people had detectable B-cell levels, compared to about 33% of white people.
Exactly why this is happening isn’t understood yet, but genetic differences that affect the immune system may play a role, Silverman said.
Black people tend to have more aggressive MS, and more research in larger groups of people is needed to determine whether this faster return of B-cells means they are more likely to have greater disease activity, he said.
“B-cells come back more quickly in Black patients treated with these drugs, so it’s important to be vigilant,” he said. “We can treat more frequently if an individual needs it.”
Immune system players known as T-lymphocytes drive the destruction in MS, he explained. “B-cells are encouraging these bad T-cells to destroy myelin, and rituximab or ocrelizumab take B-cells out of the equation, without really affecting the body’s ability to fight infection,” he explained. Many drugs that alter the immune system can increase risks for infection.
The research will be presented this week at the virtual annual meeting of the American Academy of Neurology. Findings reported at medical meetings are considered preliminary until published in a peer-reviewed journal.
Calling the new research “critically important,” Julie Fiol, the director of MS information and resources at the National MS Society, said that investigating whether Black people with MS experience the same or different responses to MS treatments as white people is a research priority.
“We know that Black people with MS experience more relapses, greater disability, and tend to require mobility assistance earlier in the disease course than whites,” she said. “We need more and larger studies to better understand if this type of therapy works differently in Black people with MS. And once we learn more, it’s possible that how much or how often someone gets a specific [drug] could change.”
More information
The National MS Society has more about MS in the Black community.
SOURCES: Gregg Silverman, MD, professor, department of medicine, NYU Langone Health, New York City; Julie Fiol, MSW, BSN, RN, MSCN, director, MS information and resources, National MS Society, New York City; American Academy of Neurology virtual annual meeting, April 17-22, 2021
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










