- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
Guidelines Aim to Detect More Congenital Heart Defects in Womb
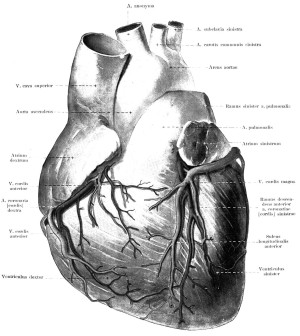

Despite advances in technology that make it much easier for doctors to detect heart defects in fetuses, more than half of babies with heart abnormalities go undiagnosed before they’re born, experts say.
A new scientific statement from the American Heart Association (AHA) seeks to improve that situation by offering updated guidelines on detecting, managing and treating heart problems in the womb.
“Congenital heart disease is the most common birth defect that can result in either death or significant health problems in newborn babies,” statement lead writer Dr. Mary Donofrio, director of the fetal heart program and critical care delivery service at Children’s National Medical Center in Washington, D.C., said in an AHA news release.
“We now have advanced imaging technologies, such as high-resolution ultrasound and three- and four-dimensional echocardiography, magnetic resonance imaging (MRI), fetal electrocardiography and magnetocardiography enabling physicians to diagnose fetal abnormalities early and with better detail and accuracy,” she noted.
“Despite this, more than half of babies with congenital heart disease go undiagnosed before birth,” Donofrio said. “We created these guidelines to provide pediatric cardiologists, obstetricians, maternal fetal specialists, radiologists, nurses and other health care providers with the latest developments in the rapidly developing area of fetal cardiology.”
The statement recommends that pregnant women with certain risk factors be referred for fetal echocardiography, which uses sound waves to examine the heart of a fetus.
A variety of women may be at higher risk of giving birth to a baby with congenital heart disease, the statement noted.
Among these are women who had diabetes before pregnancy or developed diabetes in the first trimester. In addition, taking painkillers called nonsteroidal anti-inflammatory drugs (NSAIDs) in the third trimester, having congenital heart disease or a close relative with congenital heart disease, or having other specific medical conditions are also risk factors.
Other women possibly at higher risk are those who used in vitro fertilization to get pregnant, according to the statement.
Fetuses diagnosed with a heart defect should be closely monitored and doctors should plan the care that the baby will require at and after birth, the statement advised. Some fetal heart rhythm and function abnormalities can be treated with medicines given to the mother. Surgery to correct heart problems while the baby is still in the womb are still considered experimental, the statement noted.
The statement called for health care providers to help parents and other family members deal with anxiety and depression after learning that the unborn baby has a heart defect. This can help them move from grief to acceptance.
Doctors need to be open and forthright about the problem, treatment details and likely outcomes for the children, such as whether they’ll be able to play sports and what type of physical and mental support they may need.
The guidelines in the statement, published April 24 in the journal Circulation, will provide “improved care for babies with congenital heart disease, starting in the womb and continuing after delivery and through their lives,” Donofrio said.
More information
The U.S. National Heart, Lung, and Blood Institute has more about congenital heart defects.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










