- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
Immune Protein Found to Block HIV Spread in Some People

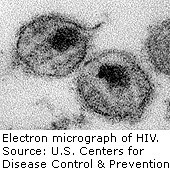
WEDNESDAY, Oct. 16One percent of people infected with HIV have a second line of defense deep in their immune system, which serves as a back-up for the body’s defenses that get wiped out by the virus, according to a new study.
These people, known as “controllers,” are able to maintain long-term control of HIV without a daily regimen of antiviral medication because of a defensive immune protein, known as A3, which blocks the virus from spreading throughout their body.
Scientists from Northwestern University suggested their findings could help shorten the drug treatment required for others who have HIV, the virus that causes AIDS.
“Preserving and even increasing this defense in cells may make more HIV-infected persons into controllers and prevent HIV from rebounding to high and damaging levels when anti-HIV medications are stopped,” the study’s senior author, Dr. Richard D’Aquila, director of Northwestern’s HIV Translational Research Center, said in a university news release.
In conducting the study, published online Oct. 16 in PLoS ONE, the researchers analyzed the cells of controllers in a lab. They found that these rare individuals have a greater supply of the A3 protein in specific white blood cells called resting memory T cells. Any new HIV made from those cells is rendered harmless by A3 and is unable to infect other cells.
Unlike other cells in the immune system that are unable to recognize HIV once it mutates, A3 is part of the so-called intrinsic immune system that isn’t fooled by the virus. “The intrinsic immune system recognizes the basic guts of the virus — the nucleic acids — that HIV can’t change and then damages those nucleic acids,” D’Aquila explained.
The researchers suggested that earlier treatment could help others eventually maintain control of their HIV without medication by protecting their reserves of A3.
“Perhaps starting anti-HIV drugs very soon after HIV is caught, rather than the current practice of waiting until later to start, would work like the controllers’ first line of defense,” D’Aquila said. “If we preserve A3, it could minimize HIV’s spread through the body as this protein seems to do in controllers.”
The researchers noted there are several cases of early HIV treatment resulting in long-term control of the virus. For example, in January 2013, a baby born to an HIV-positive woman became infected with the virus but was given anti-HIV drug treatment within 36 hours of birth. That baby is now off antiviral medication and apparently cured of HIV, D’Aquila said.
If HIV remains unchecked for several months, however, the researchers suggested reserves of A3 are simply wiped out. They are currently working to develop a drug that would boost the A3 protein.
“Early-as-possible detection — much easier with our new technology — and early drug treatment will be the future of HIV therapy,” D’Aquila concluded. He added that the new U.S. health law, the Affordable Care Act, now requires insurance companies to pay for routine HIV testing.
More information
The U.S. National Institute of Allergy and Infectious Diseases has more about treatment for HIV.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










