- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
Most Don’t Need ‘Bridging’ When They Stop Warfarin Temporarily

Heart patients on the clot-preventing drug warfarin usually have to stop the medication before having surgery. Now, a new study shows they can safely do that without taking another anti-clotting drug — and they may even be better off.
The study, reported in the Aug. 27 New England Journal of Medicine, helps answer long-standing questions about how to manage patients taking warfarin (Coumadin) for an irregular heart rhythm known as atrial fibrillation.
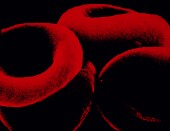
Because warfarin is a powerful anticoagulant — which means it prevents blood clots — it can also raise the risk of internal bleeding. That’s why people typically have to stop using warfarin in the days before and after an elective surgery.
But it hadn’t been clear whether those patients need what doctors call “bridging anticoagulation.” That means taking another type of anti-clotting medication that is short-acting — usually heparin.
For years, it’s been up to individual doctors and patients to decide, said Dr. Thomas Ortel, the senior researcher on the new study, and a professor of medicine at Duke University Medical Center, in Durham, N.C.
“We’ve had no clinical trial to tell us whether we need to be [bridging] at all,” Ortel explained.
Now that clinical trial is done. And, it shows that for most atrial fibrillation patients, bridging with heparin is unnecessary, Ortel said.
In fact, the study found, bridging with heparin appears to raise the risk of major internal bleeding — without any reduction in the risk of blood clots.
“For years, we’ve thought that bridging would be beneficial,” said Dr. Alfonso Tafur, a vascular medicine specialist at NorthShore University Health System, in Chicago.
“But this study shows that for the majority of (atrial fibrillation) patients, bridging puts them at unnecessary risk,” said Tafur, who was not involved in the research.
The study included nearly 1,900 patients who were having elective surgery or other invasive procedures and were taking warfarin to treat atrial fibrillation.
Atrial fibrillation is an irregular heart rhythm in which the heart’s upper chambers quiver instead of efficiently pumping blood into the lower chambers, according to the American Heart Association. It’s not immediately life-threatening, but it boosts the risk of blood clots forming in the heart. Those clots can then be pumped out of the heart and into an artery supplying the brain, causing a stroke. That’s why these patients usually take an anti-clotting drug like warfarin to prevent these clots.
A problem with warfarin is that its effects take time to kick in, and time to wear off once a person stops using it. So when warfarin patients need surgery, they typically go off the drug about five days beforehand; once they restart, it takes another five to 10 days for the warfarin to be effective again, according to background information in the study.
In this study, Ortel’s team randomly assigned patients to take either heparin or an inactive placebo during that time window.
In the end, heparin showed no effect on blood-clot risk. Just 0.3 percent of treated patients developed a clot within a month of their procedure, versus 0.4 percent of patients given the placebo, the study found.
On the other hand, heparin did boost the odds of serious bleeding. Just over 3 percent of patients developed “major” bleeding, compared with just over 1 percent of placebo patients, the study found.
The findings suggest that bridging is unnecessary for most atrial fibrillation patients, Ortel said, but there are some who still might benefit.
Tafur agreed. He said that patients who are at particularly high risk of a blood clot — such as those who’ve had a stroke in the past — might still need heparin when they go off warfarin.
For them, Tafur said, the increased bleeding risk may be offset by the anti-clotting benefit.
If your doctor does recommend bridging, Ortel said, feel free to ask why it’s necessary.
There are times when warfarin patients may not have to stop the drug at all, Tafur pointed out. With relatively simple procedures, like tooth extractions and even catheter ablation — which is sometimes used to treat atrial fibrillation — a warfarin break may be unnecessary, he said.
And what about people who are on newer clot-preventing drugs, like dabigatran (Pradaxa), rivaroxaban (Xarelto) and apixaban (Eliquis)? Those medications act differently from warfarin, Ortel said, and bridging should be unnecessary in most cases.
More information
The American Heart Association has more on treating atrial fibrillation.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










