- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
Study Compares Tissue-Based or Mechanical Replacement Heart Valves

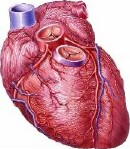
When the heart’s aortic valves cease to work properly, surgeons often use replacement valves to help restore proper cardiac function.
Now a new study compares two leading types of aortic valve replacements, and finds they have similar performance in terms of long-term risk of stroke and death for patients.
However, the study also found significant differences between the two types of devices when it came to rates of major bleeding and the need for another heart valve operation.
According to background information from the researchers, each year in the United States about 50,000 people receive an aortic valve replacement.
“Surgical aortic valve replacement is indicated for patients with symptoms of heart failure and a dysfunctional aortic valve, either too narrow or too leaky,” explained one expert, Dr. Chad Kliger, a structural heart interventional cardiologist at Lenox Hill Hospital in New York City. He was not connected to the new study.
“The types of replacement include mechanical, which are made of metal alloy disks attached by hinges, or bioprosthetic [tissue], which are made from pig or cow tissue,” he added.
In the new study, researchers led by Yuting Chiang, of Mount Sinai Hospital in New York City, analyzed data from more than 4,200 patients, aged 50 to 69, who underwent aortic valve replacement with either a bioprosthetic valve or a mechanical valve.
Reporting in the Oct. 1 issue of the Journal of the American Medical Association, they found that survival rates after 15 years were about 61 percent in the bioprosthetic valve group and 62 percent in the mechanical valve group. Stroke rates after 15 years were also similar, at 7.7 percent and 8.6 percent, respectively.
However, the number of patients who required another heart valve operation after 15 years was about 12 percent in the bioprosthetic valve group, compared to only 7 percent in the mechanical valve group, Chiang’s group reported.
But mechanical valves had their downside, too — rates of major bleeding after 15 years were 13 percent in the mechanical valve group, but fell to 6.6 percent in the bioprosthetic valve group, the study found.
According to Kliger, the difference in bleeding rates wasn’t surprising.
“Mechanical valves require blood thinners to maintain function, placing patients at risk for bleeding complications,” he explained.
On the other hand, rates for reoperation are lower for people with mechanical valves.
“Tissue valves degenerate over time, with reoperation of contemporary valves occurring at between 10 to 15 years from implantation,” Kliger noted. But he added that in this study, only 12 percent of people who received a tissue-based replacement valve ended up needing another operation, a statistic Kliger called “comforting.”
According to the Mount Sinai researchers, in the “absence of a significant survival benefit associated with one prosthesis type over another,” decisions as to which type of valve to implant should be based on other factors, such as how much blood thinning medication the patient might need, and risks for incidents such as bleeding and the need for more surgeries.
Dr. Bruce Rutkin is interventional director of Transcatheter Valve Therapies at North Shore University Hospital in Manhasset, N.Y. He agreed that the finding on bleeding rates was unsurprising, given the higher use of blood thinners by patients who receive mechanical valves.
“The findings suggest that in this age group [50 to 69], either valve type represents a reasonable choice, but patient- and physician-specific concerns — such as the preference to avoid lifelong anticoagulation — may be taken into account when deciding on a valve type,” Rutkin said.
More information
The American Heart Association has more about heart valve problems and treatments.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










