- Comparing Whey and Plant-Based Protein: Which is Best?
- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
Few Sickle Cell Patients Receiving Beneficial Drug, Study Finds

Few U.S. adults with sickle cell anemia are getting a recommended medication that can help them manage pain, breathing problems and other debilitating symptoms, according to a new study.
Using a national database, researchers found that less than one-quarter of sickle cell patients who should have been taking a drug called hydroxyurea actually were.
“This is a medication that’s highly beneficial and yet most people aren’t getting it,” said Dr. George Buchanan, a sickle cell expert, and a professor at the University of Texas Southwestern Medical Center at Dallas, who was not involved in the new study.
Findings from the study were reported in the April 28 issue of the Journal of the American Medical Association.
Sickle cell anemia is an inherited disease that mainly affects people of African, South American or Mediterranean descent. In the United States, about one in 500 African-American children are born with the condition, according to the U.S. National Heart, Lung, and Blood Institute (NHLBI).
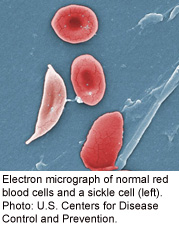
The central problem in sickle cell is that the body produces red blood cells that are crescent-shaped, rather than disc-shaped. Those abnormal cells tend to be sticky and can block blood flow — causing symptoms such as fatigue and shortness of breath.
Many people with sickle cell also suffer sudden bouts of pain due to poor blood flow. And according to treatment guidelines released last year, adults who have three or more pain “crises” within a year should be prescribed hydroxyurea.
Hydroxyurea was originally developed as a cancer drug, but it treats sickle cell by prompting the body to make fetal hemoglobin — an oxygen-carrying protein in red blood cells. That, in turn, helps keep red blood cells from becoming stiff, sticky and crescent-shaped, according to the NHLBI.
“My own view is, the vast majority of people with sickle cell anemia should be taking hydroxyurea,” said Buchanan, who helped develop the latest treatment guidelines.
He added that people who work in the field have long known that hydroxyurea is underused, but this study offers hard numbers.
“The findings are not surprising, but they’re very disappointing,” Buchanan said.
So why aren’t more people who need it getting the drug? There are several issues, said Dr. Michael DeBaun, who directs the sickle cell treatment center at Vanderbilt University in Nashville, Tenn.
For one, DeBaun explained, there are few hematologists who specialize in treating sickle cell patients — especially adults. So people with the disease often see only a primary care doctor.
But because sickle cell is relatively rare, DeBaun said, most primary care doctors have little experience treating it.
Add to that the fact that they may know little about hydroxyurea. “It’s a cancer drug,” DeBaun said, “and most internists do not go through their training learning how to manage a chemotherapy agent.”
Another issue, DeBaun said, is that many sickle cell patients are low-income blacks. Some may be uninsured or “under-insured,” and possibly have no consistent health provider. Plus, they often live in areas, whether rural or urban, that lack specialists in the disease, DeBaun explained.
For the study, Dr. Nicolas Stettler and colleagues at the Lewin Group in Falls Church, Va., used a database with information on almost 27 million Americans’ health insurance claims.
The researchers identified nearly 700 adults with sickle cell who fit the criteria for taking hydroxyurea. But based on their records, only 23 percent were using the drug within a year of their last pain crisis.
And that figure, Stettler said, may actually be an underestimate of the problem, because it doesn’t account for sickle cell patients on Medicaid or the uninsured.
The results underscore a need for education, for both doctors and patients, according to Stettler.
He suggested that people with sickle cell ask their doctor whether they should be getting hydroxyurea, or any other therapies in the treatment guidelines — which are available online.
Hydroxyurea is not without risks: It can lower the number of white blood cells and platelets in the bloodstream, which could leave people at risk of infections or bleeding. That means patients have to get periodic blood tests, Buchanan said.
But in general, he stressed, hydroxyurea is considered a safe and effective drug.
According to DeBaun, broader efforts are needed to raise awareness of existing sickle cell treatments, and spur more research into new ones. He said sickle cell patients need more-vocal advocacy groups, and more attention from policymakers.
“Care could improve if more health care resources were allocated to sickle cell,” DeBaun said.
More information
The U.S. National Heart, Lung, and Blood Institute has the latest sickle cell treatments.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










