- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Could Too Much Medication for Irregular Heartbeat Raise Dementia Risk?

People with atrial fibrillation who are overtreated with anti-clotting drugs may be doubling their risk for dementia, a new study suggests.
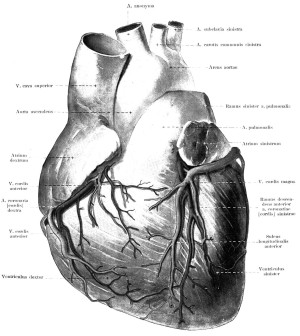
Atrial fibrillation causes the upper chambers of the heart to contract quickly and irregularly. These abnormal contractions allow blood to pool in the heart, forming clots that can cause a stroke if they break off and are carried into the brain.
However, too much anti-clotting medication may raise the chances of tiny brain bleeds that, over time, might raise the risk of dementia, the researchers said.
“In patients with atrial fibrillation, dementia risk is dependent on the efficacy and control of long-term use of anti-clotting drugs,” said lead researcher Dr. Thomas Jared Bunch, director of electrophysiology at the Intermountain Heart Institute in Murray, Utah. Warfarin and Plavix, along with aspirin, are some of the most commonly used medications for atrial fibrillation.
“Warfarin in some people is a very challenging medication to use with levels that often fluctuate between over- and under-anti-clotting,” he said.
This effect is particularly pronounced in patients who need more than one anti-clotting drug, Bunch said.
“Doctors who prescribe anti-clotting drugs have to be aware of unique long-term risks with these medications,” he said.
In those patients on warfarin where tight control is not possible, newer drugs that have more predictable effects on the body may be preferable, Bunch said.
The study findings were to be presented Sunday at the American Heart Association annual meeting in Chicago. Research presented at meetings is viewed as preliminary until published in a peer-reviewed journal.
“This is an important and underappreciated risk of atrial fibrillation,” said Dr. Sam Gandy, director of the Center for Cognitive Health at Mount Sinai Hospital in New York City. “I think that this is very important given the high prevalence of atrial fibrillation.
For the study, Bunch and colleagues studied about 1,000 patients with no history of stroke or dementia.
Over 10 years of follow-up, the researchers found that patients taking a combination of drugs who had abnormally slow clotting times 25 percent or more of the time were more than twice as likely to develop dementia as patients whose clotting time remained in normal ranges more than 90 percent of the time.
Patients who had abnormally slow clotting times were receiving too much medication, Bunch explained.
The increased risk was higher than what was found in a study of warfarin alone, he added.
Dr. Gregg Fonarow, a professor of cardiology at the David Geffen School of Medicine at the University of California, Los Angeles, said it has been thought that the increased risk of dementia in atrial fibrillation may result from the cumulative effects of many small strokes due to inadequate anti-clotting control.
“These intriguing new findings suggest that microbleeds may result in chronic brain injury and be another factor that contributes to the association of atrial fibrillation with dementia,” he said.
While the study found an association between overtreatment with anti-clotting drugs and dementia, it did not establish a cause-and-effect link.
More information
For more on atrial fibrillation, visit the American Heart Association.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










