- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
- How Daily Prunes Can Influence Cholesterol and Inflammation
- When to Take B12 for Better Absorption and Energy
- Epsom Salts: Health Benefits and Uses
Variants of COVID Virus May ‘Hide Out’ in Body: Study
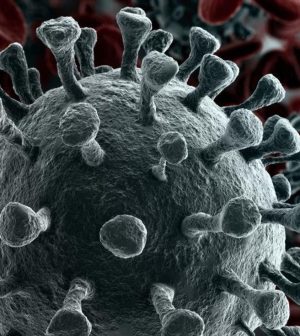
It looks like coronavirus variants can hide out in the human body much like some of their viral cousins do, making it hard for infected people to get rid of the virus entirely, researchers report.
Successive variants have appeared since the original version of SARS-CoV-2 triggered the global pandemic, and vaccines and antibody treatments have proven less effective against some of these variants.
“Our results showed that one can have several different virus variants in one’s body,” said Kapil Gupta, a senior research associate in biochemistry at the University of Bristol in the U.K. “Some of these variants may use kidney or spleen cells as their niche to hide, while the body is busy defending against the dominant virus type. This could make it difficult for the infected patients to get rid of SARS-CoV-2 entirely.”
Gupta is lead author of one of two new studies recently published in the journal Nature Communications.
The international team of researchers found that the virus can evolve distinctly in different cell types and adapt its immunity in the same infected person.
They focused on the function of a specific pocket in the SARS-CoV-2 spike protein and concluded that it plays an essential role in the virus’ ability to spread.
“An incessant series of variants have completely replaced the original virus by now, with Omicron and Omicron 2 dominating worldwide,” said team leader Imre Berger, a professor of biochemistry at University of Bristol.
Researchers analyzed an early variant discovered in Bristol dubbed BrisDelta.
“It had changed its shape from the original virus, but the pocket we had discovered was there, unaltered,” Berger explained.
BrisDelta represents a small subpopulation in samples from COVID patients, but it appears to infect certain cell-types better than the virus that dominated the first wave, researchers noted.
In a related study, researchers created synthetic, safe versions of the virus (virions) to determine how the pocket drives infection. They found that the spike protein on the virus changes shape after binding with a fatty acid. This makes it less visible to the immune system.
“It appears that this pocket, specifically built to recognize these fatty acids, gives SARS-CoV-2 an advantage inside the body of infected people, allowing it to multiply so fast,” said study author Oskar Staufer. “This could explain why it is there, in all variants, including Omicron.”
Staufer is a joint member of the Max Planck Institute in Heidelberg, Germany, and the Max Planck Center in Bristol, U.K.
“Intriguingly, the same feature also provides us with a unique opportunity to defeat the virus, exactly because it is so conserved — with a tailor-made antiviral molecule that blocks the pocket,” he added.
A company founded by the researchers is working to develop antiviral drugs that target the pocket.
More information
For more on COVID-19 variants, go to the U.S. Centers for Disease Control and Prevention.
SOURCE: University of Bristol, news release, March 1, 2022
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










