- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
Estrogen May Help Fight Severe COVID-19
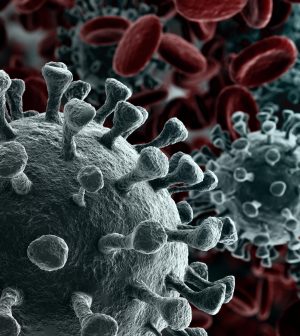
Hormone replacement therapy may offer women significant protection against dying from COVID-19, new research suggests.
British researchers who tracked more than 5,400 women with COVID during the first half of 2020 report that those who received the supplemental estrogen were 78% less likely to die within six months of their COVID diagnosis.
Nearly 5% of women in the study had been taking hormone replacement therapy (HRT) before their COVID diagnosis. HRT is used to relieve symptoms such as hot flashes and insomnia caused by lower levels of estrogen and progesterone during menopause.
“Further research would be required before we could recommend estrogen-containing medications as treatment for COVID,” said study author Christopher Wilcox. He’s an academic clinical fellow in primary care and population health at the University of Southampton.
However, he and his colleagues point out that men with COVID are more likely than women to be hospitalized and admitted to an intensive care unit. Recent data from 38 countries also indicates that men are 1.7 times more likely to die from COVID than women.
“Quite a number of studies have shown that higher estrogen levels seem to be associated with lower severity of infectious diseases, including COVID-19,” Wilcox said.
“More recently,” he added, “there have been studies suggesting that there may a protective effect from estrogen-containing medications, including HRT and the combined oral contraceptive pill.”
Still, he added, the evidence for that has not been consistent.
To learn more, Wilcox and his colleagues looked at primary care medical records drawn from a large U.K. database. Of more than 1.8 million women in that database, 5,451 had been diagnosed with COVID by the end of June 2020.
None were proactively given HRT as a treatment following their COVID diagnosis. And most had not been on hormone therapy beforehand.
But 235 patients had been on an HRT regimen during the preceding six months.
For all women, the risk of dying within six months of a COVID diagnosis was higher among those who were older, obese and/or struggling with other illnesses. Women on immunosuppressant drugs also faced a higher risk for death.
But the team determined that those on HRT faced a substantially lower risk.
Wilcox offered possible explanations. “It is thought that higher estrogen levels may be associated with increased immune responses,” he said. “Recent research suggests that this could partly explain why women have a higher and faster COVID antibody response … compared with men.”
But he stopped short of suggesting that women begin HRT after a COVID diagnosis in a bid to gain added protection.
“I certainly think women can be encouraged from these results that there is no indication to stop HRT because of the pandemic,” Wilcox said. “Further research would be required before we could recommend estrogen-containing medications as treatment for COVID.”
Dr. Thomas Gut, an associate chair of medicine with Northwell Health at Staten Island University Hospital (SIUH) in New York City, seconded that thought.
“This is not something I’ve noticed myself, but it’s interesting,” said Gut, who reviewed the study findings. “And we do know that women who have been on HRT — especially younger women — may gain some heart protective benefits. So it may be that HRT is protecting them from cardiovascular outcomes that sometimes affect COVID patients.”
But he said this kind of look-back (retrospective) study is “something that you have to take with a grain of salt, given that there are likely many variables that could influence the results that aren’t being accounted for.”
Gut, director of the SIUH Post-COVID Recovery Center, cautioned against embracing HRT as a treatment option for COVID among women not already taking it.
“There’s a strong concern any time you prescribe HRT therapy, because HRT carries significant risks,” he noted.
Those risks include an increased risk of blood clots and stroke as well as endometrial and breast cancer.
“It’s also unclear whether current usage of hormones is necessarily as helpful for COVID patients as would be prior exposure to HRT,” Gut said.
The risks of prescribing HRT as a COVID treatment would extend to both women and men — especially men, he said.
“It’s not clear whether men would benefit, and giving them HRT would expose them to risks, such as blood clots, that they wouldn’t normally encounter,” Gut said.
The findings were published May 17 in the journal Family Practice.
More information
The U.S. Centers for Disease Control and Prevention has more about COVID-19 treatments.
SOURCES: Christopher Wilcox, BSc, MBBCh, DCH, academic clinical fellow, University of Southampton, U.K.; Thomas Gut, DO, associate chair, medicine, Northwell Health, Staten Island University Hospital (SIUH), and director, SIUH Post-COVID Recovery Center, New York City; Family Practice, May 17, 2022
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










