- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Scientists Spot New Clues to a Deadly Lung Disease
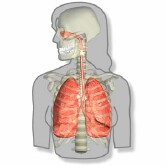
Scientists believe they’ve found a key biological player in idiopathic pulmonary fibrosis (IPF), a uniformly fatal lung disease that kills thousands of Americans each year.
The finding may be another step forward for patients who have typically had a bleak prognosis. Last month, studies revealed that two new medications might offer some hope for the first effective treatment of IPF.
Without a lung transplant, IPF remains an incurable, progressive disease that causes tissue deep in the lungs to stiffen and scar. Seventy percent of patients die within five years.
According to the Coalition for Pulmonary Fibrosis, more than 128,000 Americans suffer from IPF, with 40,000 dying from the disease each year.
The disease starts with shortness of breath or a dry, hacking cough, but soon robs the person’s body of the oxygen needed to move about or properly function, according to the U.S National Institutes of Health. Doctors don’t know what causes IPF, although they suspect that smoking, genetics, certain viral infections or acid reflux could play a role in damaging the lungs, the NIH said.
In the new study, researchers found that chronically high levels of an injury-repair protein called chitinase 3-like-1 (CHI3L1) seems linked to an accumulation of scar tissue in the lungs of people with IPF.
“The CHI3L1 is doing exactly what it is supposed to do — it is designed to shut off cell death and decrease injury,” study co-senior author Dr. Jack Elias, dean of medicine and biological sciences at Brown University, explained in a university news release.
According to Elias’ team, CHI3L1 is produced in response to injuries to lung tissue. The protein helps shield injured cells from dying, and at the same time it helps spur tissue repair — fibrosis — to “patch up” the damage. But this mechanism appears to get out of control, so stiff, fibrotic tissue keeps piling up.
“At the same time [the protein] is decreasing cell death it is driving the fibrosis,” Elias said. ” You’ve got this ongoing injury so you’ve got these ongoing attempts to shut off injury, which stimulate scarring.”
The findings came about after the multi-center team of researchers compared tissues and blood from patients with IPF against those of healthy patients. Those biopsies showed consistently elevated rates of CHI3L1 in the IPF group, but not in others.
“This demonstrates that the CHI3L1 plays a key role in controlling lung injury in this setting,” Elias said.
The findings were further corroborated in studies in mice. The rodents were first manipulated to develop an IPF-like condition. When CHI3LI protein levels were high, the mice showed evidence of accelerated scarring of lung tissue, the team said.
While not all studies conducted in the lab or in mice translate to success in humans, the new research “lays the foundation” for efforts to develop new treatments for IPF, Elias said.
“To my knowledge this is the first comprehensive paper that’s been able to explain the many facets and presentations of IPF,” he added. “It explains and links the injury and the repair responses that are critical in the disease. It also provides an explanation for the slowly progressing patients and the patients that experience acute exacerbations.”
The study was published June 11 in the journal Science Translational Medicine.
The news comes on the heels of two papers published in May in the New England Journal of Medicine. Those studies found that two drugs, pirfenidone and nintedanib, appear to slow the advance of IPF.
“It is an optimistic time for patients with fibrosis,” Dr. Gregory Cosgrove, chief medical officer for the Pulmonary Fibrosis Foundation, said at the time of the studies’ release.
“It’s been frustrating when we have not identified an effective therapy over the past 10 to 15 years,” he said. “But that degree of frustration has prompted the IPF community to really come together to support participation in clinical trials, and those trials have provided a foundation for these new advances.”
More information
The U.S. National Heart, Lung, and Blood Institute has more about idiopathic pulmonary fibrosis.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










