- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
Two-Fifths of Americans With COPD Live Far From Lung Rehab
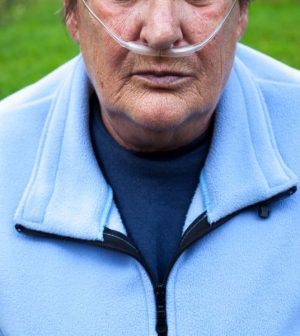
Pulmonary rehab can improve the quality of life for people with chronic obstructive pulmonary disease (COPD), but as many as 40% of U.S. seniors with COPD lack access to these programs, largely because there are none nearby.
COPD is an umbrella term for chronic lung diseases such as bronchitis and emphysema that make it harder to breathe. Often smoking-related, COPD has no cure, and treatments typically include medications to ease breathing. More than 16 million Americans are living with its debilitating effects, according to the American Lung Association.
Pulmonary rehabilitation programs — which include exercise and disease education — help supplement treatment. Classes typically meet two to three times a week for four to 12 weeks or more. Sessions can be home- or hospital-based.
But when researchers matched the ZIP codes of 10.3 million Medicare beneficiaries who were diagnosed with COPD between 1999 and 2018 with those of about 1,700 pulmonary rehab centers, they found that many patients live too far away from them to take advantage of the benefits.
In all, only 61.5% had a rehab center within 10 miles of their home, the study found. Seventy-four percent had one within 15 miles; nearly 87% had one with 25 miles, and 97% had one only within 50 miles.
“Due to limited access and awareness, people with COPD are not necessarily receiving the benefits of pulmonary rehabilitation,” concluded study author Dr. Gargya Malla, a doctoral student in epidemiology at the University of Alabama at Birmingham.
Previous research found that patients who live more than 10 miles from a pulmonary rehab center are less than half as likely to enroll as those who live closer, Malla explained.
Access is even worse in small towns and rural areas, the study showed.
A quarter of people with COPD live in small cities, small towns or rural areas, which had about one rehab center for every 4,300 COPD patients. In metro areas, about 73% of people with COPD had a pulmonary rehab center within 10 miles, compared with slightly more than 38% in smaller cities and about 17% in small towns or rural areas.
The findings were presented Tuesday at an online meeting of the American Thoracic Society. Research presented at medical meetings is considered preliminary until published in a peer-reviewed journal.
COPD experts are increasingly concerned about lack of access to these programs.
Pulmonary rehab can save lives, said Dr. Barry Make, director of the COPD program at National Jewish Health in Denver.
“It’s more than just walking or biking, it’s also strengthening and providing education about eating well, taking medications appropriately and knowing when to see a health care provider because you have a COPD exacerbation so you can treat it early and don’t wind up in a hospital,” Make said.
The quality of life benefits of pulmonary rehab are substantial, said Dr. E. Neil Schachter, a professor of medicine, pulmonary, critical care and sleep medicine at Mount Sinai Hospital in New York City.
“These programs take patients who have great limitations in everyday activities and help them get to the point where they have a quality of life that they didn’t have before,” he said.
Will they be able to run a marathon? Not likely, but Schachter said, “they won’t need oxygen when they shower or will be able to do housework.”
Schachter said he was not surprised by the new findings.
“There are so few programs and so little push to enroll patients because they are not money-making operations,” Schachter said. “Increasing the rate at which they are paid for by insurers and promoting the benefits may improve access.”
Make said a hybrid model in which some sessions are done via telemedicine and others are done in person may help more people benefit from these programs.
The COVID-19 pandemic forced many rehab programs to close — and people with long-haul COVID may need the help, both lung experts said.
“Many of the survivors of COVID are left with damaged lungs and do not recover their former lung function,” Schachter said. “The long COVID may be a source of long-term respiratory disability that will require rehabilitation and pulmonary rehabilitation will probably be the path to their recovery.”
More information
The American Thoracic Society and the Gawlicki Family Foundation have more about pulmonary rehabilitation.
SOURCES: Gargya Malla, MBBS, MPH, doctoral candidate, Department of Epidemiology, University of Alabama, Birmingham; Barry Make, MD, director, COPD program, National Jewish Health, Denver; E. Neil Schachter, MD, professor, medicine, pulmonary, critical care and sleep medicine, Mount Sinai Hospital, New York City; American Thoracic Society, online presentation, May 18, 2021
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










