- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Scientists Inch Closer to Alzheimer’s Origins
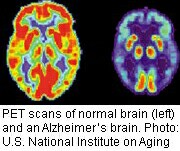
A laboratory study seems to support the theory that a buildup of beta-amyloid plaques in the brain is the first step in a process that leads to Alzheimer’s disease.
Researchers also pinpointed the important role of a particular enzyme in this process, and they believe the enzyme could offer a target for new drugs to fight Alzheimer’s.
The theory that accumulation of beta-amyloid plaques triggered Alzheimer’s disease was first suggested in the mid-1980s.
“One of the biggest questions since then has been whether beta-amyloid actually triggers the formation of the [fiber-like] tangles that kill neurons,” study co-senior author Rudolph Tanzi, director of the Genetics and Aging Research Unit at Massachusetts General Hospital, explained in a hospital news release.
According to the researchers, scientists have been stymied in the past by laboratory cell cultures that can’t replicate the “gelatinous” 3-D environment of the brain. They say their new approach gets closer to replicating that environment.
After growing special neural stem cells in the laboratory for six weeks, Tanzi’s team noticed that cells tied to a fast-progressing form of Alzheimer’s disease not only boosted levels of beta-amyloid, they also contained the “neurofibrillary tangles” that are the other hallmark of the disease.
“In this new system that we call ‘Alzheimer’s-in-a-dish,’ we’ve been able to show for the first time that amyloid deposition is sufficient to lead to tangles and subsequent cell death,” Tanzi said.
The researchers also found that boosting levels of a particular enzyme appeared to help reduce formation of the toxic tangles.
The findings were published online Oct. 12 in the journal Nature.
“This new [laboratory] system — which can be adapted to other neurodegenerative disorders — should revolutionize drug discovery in terms of speed, costs and physiologic relevance to disease,” Tanzi said.
“Testing drugs in mouse models that typically have brain deposits of either plaques or tangles, but not both, takes more than a year and is very costly,” he added.
“With our three-dimensional model that recapitulates both plaques and tangles, we now can screen hundreds of thousands of drugs in a matter of months without using animals in a system that is considerably more relevant to the events occurring in the brains of Alzheimer’s patients,” Tanzi explained.
More information
The U.S. National Institute of Neurological Disorders and Stroke has more about Alzheimer’s disease.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










