- Double Mastectomy May Offer No Survival Benefit to Women With Breast Cancer
- Toxic Lead Found in Cinnamon Product, FDA Says
- Certain Abbott Blood Sugar Monitors May Give Incorrect Readings
- Athletes Can Expect High Ozone, Pollen Counts for Paris Olympics
- Fake Oxycontin Pills Widespread and Potentially Deadly: Report
- Shingles Vaccine Could Lower Dementia Risk
- Your Odds for Accidental Gun Death Rise Greatly in Certain States
- Kids From Poorer Families Less Likely to Survive Cancer
- Tough Workouts Won’t Trigger Cardiac Arrest in Folks With Long QT Syndrome
- At-Home Colon Cancer Test Can Save Lives
Certain Rheumatoid Arthritis Drugs May Also Protect Patients’ Hearts, Studies Find

SATURDAY, Oct. 26Drugs that people with rheumatoid arthritis use to help ease the symptoms of the disease might also help ward off heart trouble, two new studies find.
Researchers in Sweden found that so-called “biologic” drugs, known as tumor necrosis factor inhibitors, or anti-TNFs, slightly reduce the risk for acute coronary syndrome — a condition that includes angina and heart attack in which blood supply to the heart muscle is suddenly blocked.
In another study, British scientists also found taking these drugs was associated with a lower risk for heart attack in patients with rheumatoid arthritis.
The findings were to be presented Saturday at the American College of Rheumatology’s annual meeting in San Diego. Findings presented at medical meetings are typically considered preliminary until published in a peer-reviewed journal.
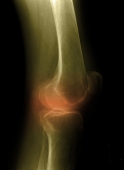
The roughly 1.3 million Americans affected by the rheumatoid arthritis, a disease that occurs when the immune system mistakenly begins to attack the joints, often suffer from pain, stiffness, swelling, and have trouble moving and using many of their joints. The condition, which is twice as common among women, can also cause inflammation in the organs.
One expert said heart problems were also an issue for many patients.
“It has been known that patients with rheumatoid arthritis have a greater risk of developing heart disease than those without,” said Dr. Kenneth Ong, acting chief of cardiology at The Brooklyn Hospital Center in New York City. “This risk seems to extend in many forms of cardiovascular disorders, among which the most notable is coronary artery disease, but also includes heart failure, peripheral artery disease and possibly stroke.”
For the past decade, anti-TNF drugs have been used around the world to treat rheumatoid arthritis as well as other inflammatory conditions. These pricey medications — prescribed under brand names such as Remicade, Enbrel, Humira, Cimzia and Simponi — have been shown to reduce inflammation.
In the first study, the Swedish team compared rates of heart disease among patients with rheumatoid arthritis taking anti-TNFs with patients not using the drugs and people in the general population, to see if the medications could also cut the risk for heart issues.
The study involved a group of more than 7,700 patients in Sweden with rheumatoid arthritis who had never been diagnosed with heart disease. They began taking anti-TNFs between 2001 and 2010. Of this group, about 76 percent were women averaging about 57 years of age. The researchers compared these patients to a group of more than 23,000 similar people who also had rheumatoid arthritis but had never taken anti-TNFs, as well as a group of more than 38,500 similar people randomly selected from the general population in Sweden.
The researchers classified exposure to the drugs into three categories: those who were “actively” on the drugs; those with “short-term exposure” who took the medication for up to two years; and those who had “ever” taken the medication at some point.
The study revealed the prevalence of heart events was slightly lower among patients with rheumatoid arthritis who were actively taking anti-TNFs than people with rheumatoid arthritis who had never taken this type of medication. Patients actively taking anti-TNFs were 50 percent more likely to have angina or heart attacks than the general population, while patients who had never taken these medications were more than twice as likely to have these heart events.
After taking other factors into account, such as how long the patients had rheumatoid arthritis, other diseases affecting the patients and socio-economic status, the researchers found that patients actively on the drugs had a 27 percent lower risk for angina/heart attack than patients who had never taken such a drug.
“This nationwide study adds to the evidence that use of TNF inhibitors for rheumatoid arthritis also has an impact on cardiovascular [illness],” study author Dr. Lotta Ljung, a senior consultant in rheumatology at Umea University Hospital, said in a news release issued by the meeting organizers.
However, she stressed that it’s not clear whether the drugs themselves caused the lowering of heart risks, or whether an easing of rheumatoid arthritis was the underlying cause of better heart health.
A second study conducted by researchers in the UK examined the effects of anti-TNF drugs on patients’ risk for heart attacks. The researchers compared use of these drugs among patients with rheumatoid arthritis to patients taking more traditional drugs, known as non-biologic disease-modifying antirheumatic drugs (DMARDs).
Using The British Society for Rheumatology Biologics Register, which contains information compiled between 2001 and 2008 on more than 20,000 patients in the UK, the researchers examined the rate of heart attacks among nearly 14,300 people with rheumatoid arthritis. They also considered whether the severity of heart attacks was in any way affected by treatment with TNF inhibitors.
The researchers also used data from two previous British studies. One examined the safety of biologic drugs, the other examined heart attack-related hospitalizations in England and Wales.
“Better control of inflammation with biologic therapy might reduce not only the rate of heart attacks, but potentially also affect the size of [heart attacks],” reasoned study co-author Dr. William Dixon a rheumatologist with Arthritis Research UK’s Epidemiology Unit at the University of Manchester.
The study showed that patients taking anti-TNF drugs were at lower risk for heart attack than patients taking traditional DMARDs. However, use of the biologic drugs did not affect the severity of heart attacks, the British team found.
In the news release, Dixon said that “rheumatologists can be reassured that treatment of active rheumatoid arthritis with anti-TNF therapy may lead not just to an improvement in joint symptoms, but also a reduction in the rate of [heart attacks] in the medium term.”
His team pointed out, however, that patients with rheumatoid arthritis generally have an increased risk of heart attacks. So, even though anti-TNFs may help curb the risk for heart attacks they do not eliminate it. The U.K. group conclude that patients with rheumatoid arthritis who taking biologic drugs still need to take steps to cut their risk for heart disease.
One expert not connected to the studies agreed.
“Given that these studies demonstrate the increased risk of cardiovascular disease in rheumatoid arthritis, patients should try to mitigate other known cardiovascular risk factors by not smoking and maintaining a healthy diet and weight,” said Dr. Diane Horowitz, a rheumatologist at North Shore University Hospital in Manhasset, N.Y., and Long Island Jewish Medical Center in New Hyde Park, N.Y.
For his part, Ong said it makes “sense that drugs that reduce inflammation in rheumatoid arthritis could reduce some of the risk of developing heart disease in these same patients.”
But he added that the studies also raise intriguing questions, such as whether or not the heart-healthy benefits of anti-TNFs last beyond the time of treatment, whether the benefit extends equally to men and women and whether these results extend to patients who do not require hospitalization for heart issues.
Cost was another issue, Ong said. “Anti-TNF drugs are among the most expensive medications developed for the treatment of rheumatoid arthritis,” he said. “I understand that it is not the first line of treatment for rheumatoid arthritis [but] if these initial results are verified by subsequent studies, the cost of treating rheumatoid arthritis may skyrocket.”
More information
The U.S. National Institute of Arthritis and Musculoskeletal and Skin Diseases provides more information on rheumatoid arthritis.
Source: HealthDay
Copyright © 2024 HealthDay. All rights reserved.










