- Vaping Linked to Earlier Onset of Asthma
- FDA Approves New Drug for Deadly Lung Cancer
- U.S. Justice Department Moves to Reclassify Weed as Less Risky Drug
- Global Life Expectancy Could Rise By More Than 4 Years by 2050
- Most Cancer Treatments Near End of Life Are Useless: Study
- Brain’s ‘Food Smell’ Circuitry Might Drive Overeating
- The More Kids Use Social Media, The More They’re Likely to Vape
- Men Are More Debilitated by Diabetes Than Women
- Is Your Child Ready for Summer Sleepaway Camp?
- Leptospirosis: What Every Dog Owner Should Know
FDA OKs High-Tech Diabetes Device to Help Replace Fingerstick Tests
In news that’s sure to delight people with diabetes, the U.S. Food and Drug Administration said Tuesday that the Dexcom G5 continuous glucose monitoring system (CGM) can be used to make insulin dosing decisions alone, without the need for additional fingerstick tests of blood sugar levels.
That means people with diabetes who use the Dexcom G5 CGM will likely be spared at least three or four fingersticks a day. Right now, blood sugar tests require the use of a lancing device to prick a small hole in the finger to collect a drop of blood to measure the current blood sugar level.
And, until now, even people with a continuous glucose monitor needed to verify those levels before figuring out how much insulin they needed for meals, or to bring down a high blood sugar level. Now, they’ll just need to do two fingersticks a day (once every 12 hours) to be sure the Dexcom CGM device is calibrated properly, and giving correct readings.
More than 29 million people have diabetes, according to the U.S. Centers for Disease Control and Prevention.
People with type 1 diabetes don’t make enough insulin — a hormone the body needs to use the carbohydrates in food for fuel. Because of this, people with type 1 rely on insulin injections or insulin delivered through a tiny catheter inserted under the skin and then attached to an insulin pump worn outside the body. People with type 1 diabetes may need five or six insulin injections daily.
In people with type 2 diabetes, the body is no longer able to use insulin properly. Most (95 percent) of diabetes cases involve the type 2 form of the disease.
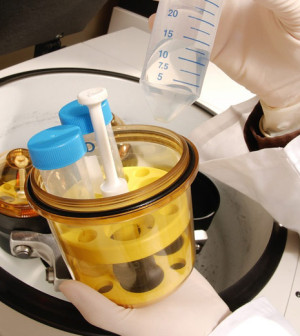
To measure blood sugar levels, the Dexcom G5 CGM relies on a small sensor wire inserted just below the skin. This wire continuously monitors blood sugar levels and, through a transmitter worn on the skin, sends information on blood sugar levels to a dedicated receiver, and a compatible mobile device — such as a smartphone or a tablet.
When blood sugar levels go out of range — either too high or too low — the receiver and the mobile device will send an alarm, alerting the person with diabetes (or a parent for babies and children with diabetes) to the problem.
This is important because when blood sugar levels drop too low, people with diabetes can become disoriented, and if levels drop even further, they may pass out. And, over time, blood sugar levels that are too high and left untreated can cause complications, such as kidney troubles, eye problems and heart disease.
If readings from the device are off, risks include blood sugar levels that are too high or too low, and potentially incorrect insulin dosing, the FDA said.
The Dexcom G5 is the first continuous glucose monitoring system to receive FDA approval for insulin dosing decisions.
“Although this system still requires calibration with two daily fingersticks, it eliminates the need for any additional fingerstick blood glucose testing in order to make treatment decisions. This may allow some patients to manage their disease more comfortably,” said the FDA’s Alberto Gutierrez. He directs the Office of In Vitro Diagnostics and Radiological Health in the FDA’s Center for Devices and Radiological Health.
These real-time blood glucose readings can also help providers and people with diabetes to see trends in blood sugar levels that can aid in better diabetes management, the FDA said in a news release.
The FDA used the results from two clinical studies before granting approval to the Dexcom G5 CGM for treatment decisions. These studies included 130 children with diabetes who were 2 or older. No serious adverse events were reported in these studies.
“The FDA works hard to help ensure that novel technologies, which can reduce the burden of daily disease management, are safe and accurate,” Gutierrez said.
More information
Learn more about continuous glucose monitoring from the U.S. National Institute of Diabetes and Digestive and Kidney Diseases.
Source: HealthDay
Copyright © 2024 HealthDay. All rights reserved.










