- Comparing Whey and Plant-Based Protein: Which is Best?
- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
Half of Diabetes Patients on Ozempic, Mounjaro Stop Using the Meds
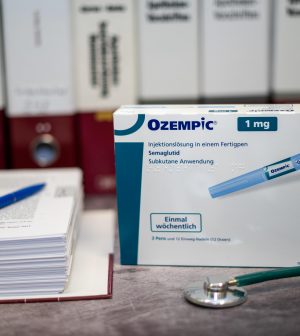
Many Americans battling diabetes are turning to a new class of injected drugs that includes blockbusters like Ozempic (semaglutide) and Mounjaro (tirzepatide).
But a new study finds half of patients who use these “second line” therapies — a class called GLP-1 RAs — quit them within a year.
The main factor: Gastrointestinal issues like nausea, vomiting and diarrhea, according to the researchers.
“Discontinuation is bad. It is common in all five types of [diabetes] medications, but we see significantly more in those prescribed the GLP-1 RAs,” said study lead author David Liss. He’s a research associate professor of general internal medicine at Northwestern University Feinberg School of Medicine in Chicago.
The study was published Dec. 12 in the American Journal of Managed Care.
People newly diagnosed with type 2 diabetes are typically first given a standby medication, metformin, to help manage their blood sugar.
But sometimes metformin isn’t enough, and patients then migrate to a second-line therapy, such as a GLP-1 RA.
Besides Mounjaro and Ozempic, this class includes exenatide (Byetta), liraglutide (Saxenda) or dulaglutide (Trulicity).
In the new study, Liss’ group tracked prescription adherence for more than 82,000 diabetes patients tracked between 2014 and 2017.
They looked at people taking one of five classes of diabetes meds (excluding insulin). In four of the five classes, about 38% of people stopped taking the drug within a year of switching away from metformin, the study found.
However, that number rose to 50% among those who’d been switched to a GLP-1 RA, the researchers noted.
“Presumably, the doctor is saying, ‘You need to start a new medication to control your type 2 diabetes,’ and then within a year, half of them just stop and don’t start another one, and that’s not a good thing,” Liss said in a Northwestern news release.
The study wasn’t designed to pinpoint why folks quit the drugs, although gastrointestinal side effects probably play a role, the researchers said.
Those issues can also arise when folks without diabetes take a GLP-1 RA for weight loss.
Two newly approved GLP-1 RA medications — Wegovy (a different form of semaglutide) and Zepbound (a different form of tirzepatide), are designed for weight loss.
“We know there are gastrointestinal side effects for these drugs that are currently in the news, both for patients with diabetes and patients attempting to lose weight,” Liss said.
Quitting a GLP-1 RA med doesn’t necessarily mean an immediate spike in blood sugar, “but discontinuation still puts these patients at greater risk for downstream hospitalizations related to diabetes,” Liss warned.
His team worry that many patients may stop using their GLP-1 RA without mentioning it to their physician. That’s a potentially dangerous move.
“Our results may represent a ‘wake-up call’ for clinicians that many of their patients were not taking the medicines that were prescribed,” Liss said. “While we don’t know if providers were aware of the discontinuation events observed in this study, our results highlight the need for ongoing communication between patients and prescribers over time — around medication benefits, side effects and costs — not just at the time of prescribing.”
More information
Find out more about this class of medications at the Mayo Clinic.
SOURCE: Northwestern University, news release, Dec. 12, 2023
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










