- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Mouse Study Suggests Antibiotics May Aid Salmonella’s Spread in Animals

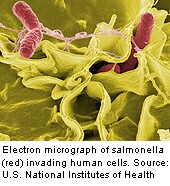
Antibiotics might actually help Salmonella — bacteria that cause food poisoning — spread among infected animals, according to new research.
Although this phenomenon isn’t yet known to have occurred among people, the study’s authors cautioned their findings should serve as a reminder of the potential dangers of antibiotic use.
They also noted that their findings call into question the pervasive use of low doses of antibiotics among livestock.
“We humans shouldn’t take antibiotics lightly. We need to consider whether they’re always beneficial when they’re given to animals across the board, or when we take them ourselves,” said the study’s senior author, Denise Monack, associate professor of microbiology and immunology at Stanford University School of Medicine, in a university news release.
The study’s authors explained that some mice are normally what’s known as “superspreaders.” These mice can shed feces carrying large amounts of bacteria that can infect and sicken other mice, but yet remain symptom-free themselves.
When the researchers gave the antibiotic streptomycin to mice infected with Salmonella typhimurium, they found that a small number of normal mice began to shed large quantities of bacteria in their feces, much like the superspreaders. But, unlike the superspreaders, these mice became increasingly ill, according to the study.
In a matter of hours, most of the mice that had been shedding relatively low amount of salmonella in their feces had very high levels of the bacteria in their gut and their feces. Within days, these mice developed symptoms and became sick. Several of them died, the study, published on online on Oct. 20 in the Proceedings of the National Academy of Sciences revealed.
Meanwhile, the so-called superspreaders appeared healthy and were unaffected by the infection and the antibiotic, the researchers found.
The levels of salmonella in the guts of former non-superspreaders were close to those of superspreaders, the researchers found. They noted the bacteria shed by former non-superspreader mice were just as infectious as those shed by superspreaders. That means the antibiotic treatment had the opposite effect of what it should have — increasing the risk of infection instead of reducing it, according to the researchers.
The researchers found the same results when they gave mice a different antibiotic, neomycin, according to the study.
Roughly 80 percent of all antibiotics used in the United States are given to cattle, pigs, chicken and other livestock, according to the researchers. The drugs are given to boost the animals’ growth rates, although experts have warned that this practice contributes to the increase in drug-resistant germs, the researchers explained.
“We’ve shown that the immune state of an infected mouse given antibiotics can dictate how sick that mouse gets and also carries implications for disease transmission,” said Monack. “If this holds true for livestock as well, and I think it will, it would have obvious public health implications. We need to think about the possibility that we’re not only selecting for antibiotic-resistant microbes, but also impairing the health of our livestock and increasing the spread of contagious pathogens among them and us.”
Identifying superspreaders could prevent Salmonella epidemics, but this has been difficult since they do not have symptoms. Inspecting stool samples is one way to detect superspreaders but this would be challenging when dealing with livestock, the researchers noted. The researchers noted the differences in the immune systems of superspreaders could allow them to be identified through a blood test.
Salmonella infections cause roughly 1 million cases of food poisoning each year, sending 19,000 people to the hospital, the researchers said.
More information
The U.S. National Institute of Allergy and Infectious Diseases provides more information on drug-resistant bacteria.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










