- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
Half of COVID Survivors Struggle With Depression: Study
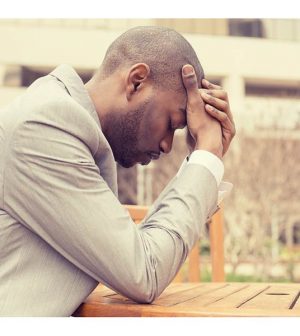
To the lingering damage of COVID-19 infection, add this side effect: New research shows that more than half of those sickened by COVID-19 report depression.
Among more than 3,900 people who had COVID-19 surveyed between May 2020 and January 2021, 52% suffered symptoms of major depression, researchers found.
“People who have been ill with COVID-19 can experience depressive symptoms for many months after their initial illness,” said lead researcher Dr. Roy Perlis. He is a professor of psychiatry at Harvard Medical School and associate chief of research in the department of psychiatry at Massachusetts General Hospital, in Boston.
The combination of chronic stress during the pandemic and disruption of people’s social networks is already a recipe for depression and anxiety, Perlis said.
“This observation reinforces the importance of understanding whether this is an effect of COVID-19 itself, or simply the stress of dealing with the pandemic plus an acute illness,” Perlis added.
The researchers also found that those with depression were more likely to be young, male and have suffered from severe COVID-19.
Earlier studies had found a connection between depression and the loss of smell and taste among COVID-19 patients, but Perlis and his colleagues did not find this relationship.
Rather, they found a link between headaches during COVID-19 and a higher risk of depression. However, it’s possible that people with depression were more likely to say they had headaches when they were sick, the study authors noted.
The study could not prove cause and effect. It’s possible that those who said they were suffering from depression had their symptoms before they had COVID-19, or that they were slower to recover from depression after being sick or were more at risk for COVID-19 in the first place, the researchers stressed.
“Depression is a very treatable illness. Because the rates of depression are currently so high, it’s especially important to ensure that people are able to access care,” Perlis noted.
“In the same way our leaders in government and public health are working to encourage people to seek vaccination, we need to encourage people to seek care if they experience symptoms of depression,” he said.
Brittany LeMonda, a senior neuropsychologist at Lenox Hill Hospital in New York City, said that the findings “are interesting, given that we are still understanding the psychiatric and neurologic manifestations of COVID-19.”
Interestingly, headache during infection, but not other symptoms, was an independent factor for depression, she said. “Individuals with a history of headache and [physical symptoms, such as pain or weakness] are often more likely to have psychiatric symptoms,” she explained.
“Underlying factors may predispose someone to develop headache with COVID-19 that also puts them at higher risk for developing depression post-illness,” LeMonda said.
People with a history of depression and anxiety were also more likely to contract COVID-19 and have a more prolonged recovery from the virus, she noted.
“People with anxiety about their health and depression are more likely to experience anxiety in general, and it may be that depression and anxiety and certain COVID-19 symptoms are bi-directionally related,” LeMonda said.
The report was published online March 12 in JAMA Network Open.
More information
For more on COVID-19 and mental health, head to the U.S. Centers for Disease Control and Prevention.
SOURCES: Roy Perlis, MD, MSc, professor, psychiatry, Harvard Medical School, associate chief, research, department of psychiatry, Massachusetts General Hospital, Boston; Brittany LeMonda, PhD, senior neuropsychologist, Lenox Hill Hospital, New York City; JAMA Network Open, March 12, 2021, online
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










