- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Mutation Helps Coronavirus Infect More Human Cells, Study Shows
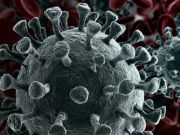
A particular mutation in one strain of the new SARS-CoV-2 coronavirus may have helped it infect more human cells and turn it into the dominant strain worldwide, new laboratory research shows.
Researchers at Scripps Research in Jupiter, Fla., stressed that their finding doesn’t mean the virus is any more lethal. And because this was research conducted in a lab, it doesn’t yet confirm that the mutation makes the strain more likely to spread among people, they added.
Still, “viruses with this mutation were much more infectious than those without the mutation in the cell culture system we used,” study senior author and virologist Hyeryun Choe, said in a Scripps news release.
Since the beginning of the global pandemic of COVID-19, experts have wondered why the virus spread relatively easily in certain areas — New York City and Italy, for example — and yet was more easily contained in other places, such as San Francisco and Washington state.
The difference may have lain in the actual structure of particular strains. The strain that’s now come to dominate underwent a mutation, dubbed D614G, that greatly increased the number of “functional spikes” on the virus’ surface.
These spikes give the virus its appearance of a “crown” (hence the name corona), and are essential in allowing the virus to latch onto human cells, causing infection, the team explained.
“The number — or density — of functional spikes on the virus is four or five times greater due to this [D614G] mutation,” Choe said.
The mutation also allowed more flexibility to the spikes’ “backbone,” Michael Farzan, co-chairman of the Scripps Research Department of Immunology and Microbiology, added in the news release. This increased flexibility helps keep the virus viable in its cell-to-cell journeys, he explained.
“Our data are very clear,” Choe said. “The virus becomes much more stable with the mutation.”
Strains of SARS-CoV-2 with the D614G mutation have grown to dominate over time. Data from GenBank, a repository for the genetic study of viral samples worldwide, found no SARS-CoV-2 sequences containing D614G in February. But by March, the mutation had appeared in one-quarter of all sequences, and by May it appeared in 70%, the team noted.
“Over time, it has figured out how to hold on better and not fall apart until it needs to,” Farzan said. “The virus has, under selection pressure, made itself more stable.”
It remains unclear whether strains carrying the D614G mutation make people any sicker or more likely to die, the researchers said. Studies conducted in hospital intensive care units show the strain to be the predominant type, but more and better data are needed, Choe and Farzan said.
The research is early: It is still undergoing peer review, but is being published in pre-print form online in bioRxiv, after news reports surfaced of the findings.
Choe and Farzan stressed that because their research was conducted using harmless viruses engineered to produce certain coronavirus proteins, it’s unclear right now whether the mutation confers increased infectivity among broad populations. Only additional studies conducted across populations can confirm that, they said.
But there was a bit of hopeful news: Immune factors derived from people infected with coronavirus did appear to battle viruses engineered with or without the D614G mutation, the team said. That bodes well for efforts to find a vaccine that can prevent SARS-CoV-2 illness, Choe and Farzan said.
One outside expert agreed that while the findings are significant, more research is needed.
Speaking with The New York Times, Michael Letko, an assistant professor in the Laboratory of Functional Viromics at Washington State University, said multiple factors can impact the spread of any virus.
“We focus on the part of the virus we know the best, the spike, but we don’t know as much about how other parts work,” he noted. The next step may be to use lab animals to test out theories regarding viral transmission.
“That’s the incredible thing about viruses,” Letko said. “They’re called Darwinian machines, and these small changes can amplify quite dramatically. These small gains can be just enough to allow a virus to outcompete another virus that doesn’t have these things.”
The work was funded by the U.S. National Institutes of Health.
More information
The U.S. Centers for Disease Control and Prevention has more on the new coronavirus.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










