- Comparing Whey and Plant-Based Protein: Which is Best?
- How Long Does Nicotine Remain in Your System?
- The Best Time of Day to Drink Bone Broth to Maximize Health Benefits
- 8 Ways to Increase Dopamine Naturally
- 7 Best Breads for Maintaining Stable Blood Sugar
- Gelatin vs. Collagen: Which is Best for Skin, Nails, and Joints?
- The Long-Term Effects of Daily Turmeric Supplements on Liver Health
- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
Scientists Discover New Way to Make Human Platelets

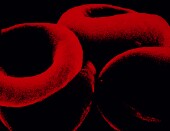
Scientists report they have discovered a new way to make fully functional human platelets, which are the blood cells that form clots.
Using human stem cells and a device called a bioreactor, which mimics the body’s natural way of producing blood cells but on a larger scale, the researchers said their method eliminates risks and complications associated with donor blood transfusion. Those include a five-day shelf-life, contamination, rejection and infection. They added that their findings could help meet increasing global demand for donor blood.
“The ability to generate an alternative source of functional human platelets with virtually no disease transmission represents a paradigm shift in how we collect platelets that may allow us to meet the growing need for blood transfusions,” study author Jonathan Thon, from the division of hematology at Brigham and Women’s Hospital in Boston, said in a hospital news release.
Blood cells, such as platelets, are made in bone marrow. The bioreactor, the researchers explained, combines the major components of bone marrow and models its composition and blood flow characteristics.
“By being able to develop a device that successfully models bone marrow represents a crucial bridge connecting our understanding of the physiological triggers of platelet formation,” study senior author Joseph Italiano Jr., of the division of hematology at Brigham and Women’s Hospital and the Vascular Biology Program at Boston Children’s Hospital, said in the news release.
The researchers hope to begin human clinical trials in 2017.
“The regulatory bar is appropriately set high for blood products, and it is important to us that we show platelet quality, function and safety over these next three years since we’ll likely be recipients of these platelets ourselves at some point,” Thon said.
One expert agreed the findings could change the way platelets are collected.
“A major factor that has limited our ability to compare bioreactor platelets to donor platelets is the inefficiency of growing platelets, a problem that slows progress of clinical research,” Dr. William Savage, medical director of the Kraft Family Blood Donor Center at Dana Farber Cancer Institute/Brigham and Women’s Hospital, said in the news release. He was not part of the study. “This study addresses that gap, while contributing to our understanding of platelet biology at the same time.”
In the United States, more than 2.17 million platelet units from donors are transfused each year to treat trauma patients and those undergoing chemotherapy, organ transplants and surgery, the researchers noted.
The study, published July 21 in the journal Blood, was partially funded by the U.S. National Institutes of Health. Thon and Italiano are co-founders of Platelet BioGenesis, a company that aims to produce donor-independent human platelets from human stem cells.
More information
The U.S. National Institutes of Health provides more information on blood transfusions and donations.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










