- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
FDA Gives Expanded Approval to Prescription Fish Oil for Heart Patients
The U.S. Food and Drug Administration on Friday gave expanded approval to a prescription form of fish oil called Vascepa, to help prevent heart trouble in people at high risk who are already taking statins.
Vascepa (icosapent ethyl) was already FDA-approved for a small percentage of patients with exceptionally high blood levels of triglycerides, a type of blood fat.
The new approval greatly expands the potential pool of patients, because it now includes people with simply high levels of triglycerides — at or above 150 milligrams per deciliter — and multiple risk factors for heart disease and diabetes.
“Today’s approval will give patients with elevated triglycerides and other important risk factors, including heart disease, stroke and diabetes, an adjunctive treatment option that can help decrease their risk of cardiovascular events,” Dr. John Sharretts said in an FDA news release. He’s acting deputy director of the Division of Metabolism and Endocrinology Products in the FDA’s Center for Drug Evaluation and Research.
Vascepa is a drug derived from fish that contains pure EPA, a key nutrient in fish oil. A month’s supply of Vascepa costs roughly $300.
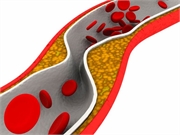
Friday’s approval follows on the positive results of a study on Vascepa presented in November at the annual meeting of the American Heart Association (AHA). Early findings from the clinical trial found that the drug slowed the development of artery-clogging plaques.
In the study, Vascepa appeared to put the brakes on key aspects of plaque formation in vessels after nine months of use, lead researcher Dr. Matthew Budoff, a professor at UCLA’s David Geffen School of Medicine, said at the time.
“We found significant slowing of progression among four different plaque markers, including total plaque,” Budoff noted in a presentation at the AHA’s annual meeting, in Philadelphia.
These early results provide some tantalizing hints why icosapent ethyl was found to reduce risk of heart-related disease and death by 25% in another study released last year, said Dr. Donald Lloyd-Jones, chair of preventive medicine at Northwestern University Feinberg School of Medicine.
EVAPORATE, the clinical trial reported on last month, is ongoing and will report final results after 18 months. Experts hope more data from the trial will show which aspect of the drug’s effect on plaque is reducing heart risk.
The EVAPORATE trial placed 40 people on high doses of icosapent ethyl and another 40 on a placebo. All participants were already taking statins and had developed at least one artery-clogging plaque. Amarin Corp., which makes Vascepa, paid for the trial.
Participants underwent CT scans at the beginning of the study and at nine months to track progression of arterial plaque in their bodies. They’ll undergo a final CT scan at 18 months.
Compared to the control group, people on icosapent ethyl experienced a slowdown in plague growth at nine months, including:
- 42% less progression in total plaque,
- 89% less new calcified plaque,
- 57% less new fibrous plaque,
- 19% less new non-calcified plaque.
Notably, the fish oil drug did not appear to actually melt away plaques, but only slowed down their growth, said Dr. Stephen Nicholls, a professor of cardiology at Monash University in Queensland, Australia.
“There was no evaporation. They all continued to progress,” said Nicholls.
There are several possible explanations why icosapent ethyl slows buildup of plaque in the arteries, Nicholls said.
The drug has been shown to reduce triglyceride levels, which contribute to plaque formation. In this study, triglycerides declined, Budoff said.
But the antioxidant and anti-inflammatory effects of the fish oil drug should also be considered as potential contributors, Nicholls said.
Newer trials have tended to support the value of fish oil drugs in controlling arterial plaques, after years of mixed results, Lloyd-Jones and Nicholls said. Both experts were not involved with the new trial.
That’s probably because earlier trials did not have people on high enough doses of purified fish oil supplements, Nicholls said.
Other high-dose fish oil clinical trials are ongoing, and will provide further evidence in the near future, Lloyd-Jones said.
More information
The Cleveland Clinic has more about fish oil and heart health.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










