- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
- Understanding the Connection Between Anxiety and Depression
- How Daily Prunes Can Influence Cholesterol and Inflammation
Prior COVID Infection Doesn’t Guarantee Good Immunity: Study
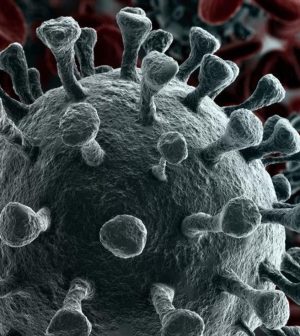
You caught a case of COVID-19 and then you got your first dose of a vaccine. Maybe you now think you are protected from coronavirus infections in the future.
Think again: New research shows that prior COVID-19 infection alone doesn’t guarantee a high level of antibodies against the coronavirus or a strong response after just one dose of two-dose vaccines.
The new study included 27 vaccinated Chicago-area adults; some had previously tested positive with the coronavirus. They submitted blood samples two to three weeks after their first and second dose of either the Pfizer or Moderna vaccines, and two months after the second dose.
Northwestern University researchers analyzed the blood samples for antibodies against the coronavirus.
“When we tested blood samples from participants collected about three weeks after their second vaccine dose, the average level of inhibition was 98%, indicating a very high level of neutralizing antibodies,” said Thomas McDade, professor of anthropology and a faculty fellow with the Institute for Policy Research.
But antibody levels against emerging variants were significantly lower, ranging from 67% to 92%.
Also, blood samples from previously infected people collected two months after the second vaccine dose showed antibody responses had declined by about 20%, according to the study published Aug. 30 in the journal Scientific Reports.
Another finding was that participants who’d had multiple COVID-19 symptoms had a stronger immune response to the vaccines than those who had mild symptoms or were asymptomatic.
“Many people, and many doctors, are assuming that any prior exposure to SARS-CoV-2 will confer immunity to reinfection. Based on this logic, some people with prior exposure don’t think they need to get vaccinated. Or if they do get vaccinated, they think that they only need the first dose of the two-dose Pfizer/Moderna vaccines,” McDade said in a university news release.
“Our study shows that prior exposure to SARS-CoV-2 does not guarantee a high level of antibodies, nor does it guarantee a robust antibody response to the first vaccine dose,” he said. “For people who had mild or asymptomatic infections, their antibody response to vaccination is essentially the same as it is for people who have not been previously exposed.”
The study was conducted before the emergence of the Delta variant, but the findings still apply, according to McDade.
“As far as protection goes after vaccination, the story is the same for all the variants, including Delta — the vaccine provides good protection, but not as good protection as the original version of the virus for which the vaccine was designed. Combine that with the fact that immunity wanes over time, you get increased vulnerability to breakthrough infection,” he said.
“So, it’s two strikes right now — Delta plus waning immunity among the first wave of the vaccinated,” McDade warned.
More information
The U.S. Centers for Disease Control and Prevention has more on COVID-19 vaccines.
SOURCE: Northwestern University, news release, Aug. 30, 2021
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










