- Could Your Grocery Store Meat Be Causing Recurring UTIs?
- Are You Making This Expensive Thermostat Error This Winter?
- Recognizing the Signs of Hypothyroidism
- 10 Strategies to Overcome Insomnia
- Could Artificial Sweeteners Be Aging the Brain Faster?
- Techniques for Soothing Your Nervous System
- Does the Water in Your House Smell Funny? Here’s Why
- Can a Daily Dose of Apple Cider Vinegar Actually Aid Weight Loss?
- 6 Health Beverages That Can Actually Spike Your Blood Sugar
- Treatment Options for Social Anxiety Disorder
Having Baby Too Soon After Weight-Loss Surgery May Raise Risks
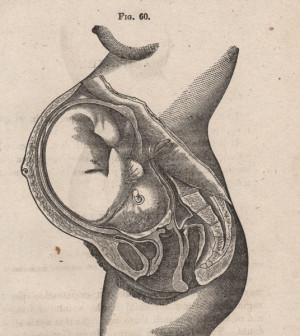
Infants born to mothers who’ve had weight-loss surgery have a higher risk for complications, and the risks are greatest for those born within two years of the surgery, a new study finds.
“A recently postoperative mother with underlying nutritional, metabolic, and physiological changes is at an elevated risk for perinatal complications,” concluded a team led by Dr. Brodie Parent, of the University of Washington Medical Center in Seattle.
One obstetrician who reviewed the findings said the issue is arising more frequently as bariatric (weight-loss) surgeries surge in popularity.
“I have been acutely aware of the recent increase in patients who have had bariatric procedures,” said Dr. Brian McKennna, who directs gynecology at Northwell Health’s Southside Hospital in Bay Shore, N.Y.
“Many of these patients have had serious nutritional deficits even before their surgery,” he added, and following the surgery, “balancing the nutritional needs of pregnancy presents unique challenges.”
In the new study, Parent’s team tracked outcomes for infants born to more than 1,800 mothers who were, on average, 29 years old. The women had all undergone weight-loss surgery less than two years or more than four years before they gave birth.
That data was compared to outcomes for infants born to more than 8,400 mothers who did not have weight-loss surgery.
Compared to infants of mothers who didn’t have weight-loss surgery, infants born to mothers who did were at higher risk for prematurity (8.6 percent vs. 14 percent), neonatal ICU admission (11 percent vs. 15 percent), and being underweight (8.9 percent vs. 13 percent).
The amount of time elapsed between the surgery and the birth seemed to matter, the Seattle researchers noted.
For example, compared to infants of mothers who had weight-loss surgery more than four years before giving birth, infants of mothers who had the surgery less than two years before giving birth were at higher risks for:
- prematurity (12 percent vs. 17 percent),
- neonatal ICU admission (12 percent vs. 18 percent),
- and being underweight (9 percent vs. 13 percent).
Parent’s group stressed that the study does not conclude that obese women who’d like to have children should reject weight-loss surgery.
“Undoubtedly, bariatric operations result in many health benefits for morbidly obese women of childbearing age and reduce obesity-related obstetrical complications,” the researchers wrote in the study. “Findings from this study should not deter bariatric surgeons from offering such therapy to this population.”
McKenna agreed, saying that women and their physicians should work together to ensure that moms-to-be’s nutritional needs, and their baby’s, are being met during pregnancy. That’s especially true for women who’ve undergone bariatric surgery, he said.
“We need to maximize a safe and nurturing environment for babies, and the first step is to help expectant mothers to achieve nutritional support and balance early on,” McKenna said. “Bariatric surgery is the beginning of a long process of healing and restoration toward normal physiology. It would be wise to counsel our patients to allow adequate time for their bodies to re-balance after these procedures.”
Dr. Mitchell Roslin, chief of obesity surgery at Lenox Hill Hospital in New York City, agreed that timing is key to minimizing any risks to pregnancy following weight loss surgery.
“We usually suggest that patients are weight-stable and nutritionally replete before attempting pregnancy — in our practice, 18 months,” Roslin said.
“With proper education, patients can remain nutritionally replete even after aggressive bariatric procedures,” he added. “Healthy women make healthy mothers.”
The study was published online Oct. 19 in the journal JAMA Surgery.
More information
The U.S. National Institute of Diabetes and Digestive and Kidney Diseases has more on weight loss surgery.
Source: HealthDay
Copyright © 2026 HealthDay. All rights reserved.










